Acetaminophen Safety: How to Avoid Overdose and Protect Your Liver
 Dec, 4 2025
Dec, 4 2025
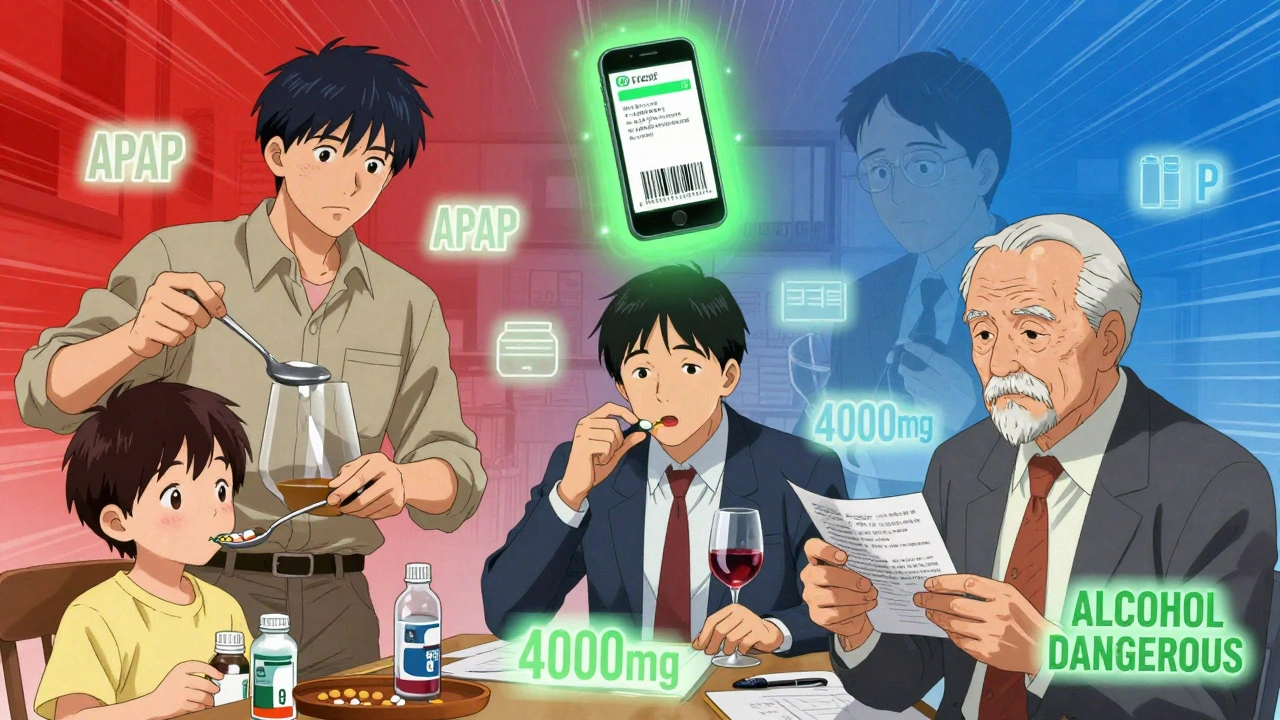
Every year, thousands of people end up in emergency rooms not because of a fall, accident, or infection-but because they took too much of a medicine they thought was harmless. Acetaminophen is in more than 600 over-the-counter and prescription products. It’s in your cold medicine, your headache pill, your sleep aid, and even some prescription painkillers. Most people don’t realize they’re stacking doses. And that’s exactly how overdoses happen.
What Acetaminophen Does-and How It Can Hurt You
Acetaminophen, also known as paracetamol or by the brand name Tylenol, is one of the most common pain and fever relievers in the world. It’s gentle on the stomach, unlike ibuprofen or aspirin, which is why doctors often recommend it for people with ulcers, kidney issues, or heart conditions. But here’s the catch: your liver has to process it. And it only has so much capacity.
At normal doses-up to 4,000 milligrams per day for adults-it’s safe. But when you exceed that, your liver can’t keep up. It starts producing a toxic byproduct called NAPQI. Normally, your body neutralizes it with glutathione, an antioxidant. But too much acetaminophen drains those stores. Without enough glutathione, NAPQI starts destroying liver cells. This isn’t a slow process. It can begin within hours.
By the time you feel sick, it might already be too late. Unlike a heart attack or a broken bone, liver damage from acetaminophen doesn’t scream for attention. You might just feel tired, nauseous, or a little off. That’s why so many people wait too long to get help.
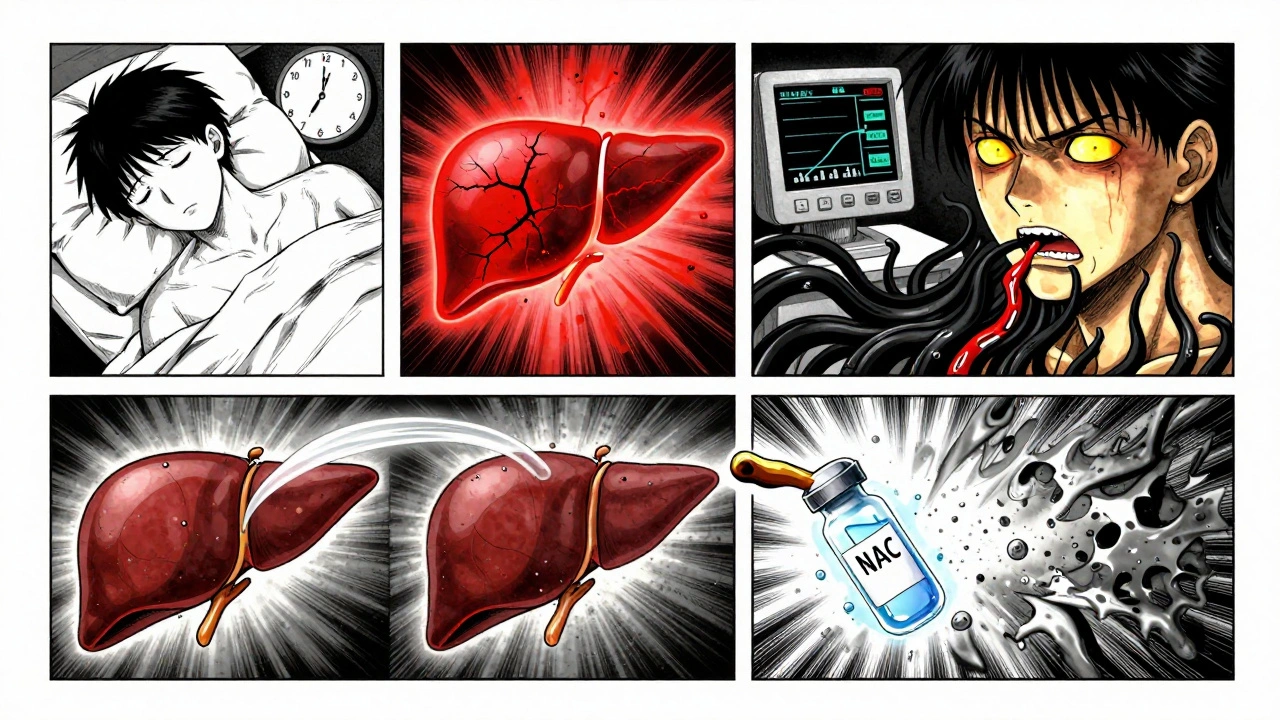
The Four Stages of an Overdose (And Why Timing Matters)
Acetaminophen toxicity doesn’t hit all at once. It unfolds in four stages, and knowing them could save your life-or someone else’s.
Stage 1 (0-24 hours): You might feel fine. Or you might have mild nausea, sweating, or a loss of appetite. Blood tests still look normal. This is the window where most people think, “I’m okay, I’ll just sleep it off.” Don’t.
Stage 2 (24-72 hours): This is when things start turning serious. Pain in your upper right abdomen-right under your ribs-becomes noticeable. Your liver enzymes (AST and ALT) begin climbing. Vomiting gets worse. You might feel dizzy or confused. This is the point where people finally go to the ER. But even here, recovery is still possible-if you get treatment fast.
Stage 3 (72-96 hours): This is the peak. Liver enzymes can spike above 10,000 IU/L (normal is under 40). Jaundice sets in-your skin and eyes turn yellow. Your blood can’t clot properly. Your kidneys start failing. About half of patients in this stage develop acute liver failure. This is where deaths happen.
Stage 4 (after 5 days): Either your liver begins to repair itself, or you don’t survive. If you get the antidote, N-acetylcysteine (NAC), within 8 hours of taking too much, your chance of full recovery is over 90%. After 16 hours, it drops to 60%. After 24? It’s a coin flip.
How People Accidentally Overdose (And How to Avoid It)
Most acetaminophen overdoses aren’t intentional. They’re mistakes. Here’s how they happen:
- You take Tylenol for a headache, then take a cold medicine that also has acetaminophen. Two doses. You don’t know.
- You’re on Vicodin or Percocet for back pain. Both contain acetaminophen. You take extra Tylenol on top. Three doses.
- You’re giving your child children’s Tylenol, but use a kitchen spoon instead of the dropper. A tablespoon isn’t a teaspoon. You’ve just doubled the dose.
- You drink alcohol regularly-even just a couple of drinks a day-and take your usual dose of acetaminophen. Alcohol makes your liver more vulnerable.
- You take extra-strength tablets (650 mg each) and think, “Four is fine,” not realizing that’s already 2,600 mg. Add another pill and you’re at the limit.
Here’s what you need to do to stay safe:
- Know the numbers. Never take more than 3,000-4,000 mg in 24 hours. If you have liver disease, don’t exceed 2,000 mg. Less is safer.
- Read every label. Look for “acetaminophen” or “APAP.” It’s not always obvious. Cold medicines, sleep aids, and even some migraine pills hide it in small print.
- Never mix with alcohol. Even one drink a day increases your risk. If you drink regularly, avoid acetaminophen entirely.
- Use the right measuring tool. For kids, always use the syringe or cup that comes with the medicine. Never guess with a kitchen spoon.
- Track your doses. Write down when you took what. If you’re on multiple meds, keep a list. Don’t rely on memory.
Why Labels Don’t Work (And What Needs to Change)
The FDA requires a “Liver Warning” on acetaminophen packaging. But studies show only 38% of people actually understand what it means. The word “acetaminophen” is tiny. The abbreviation “APAP” is confusing. The warning is buried next to inactive ingredients.
Consumer groups have been pushing for years to make the name bigger, bolder, and easier to spot. Some countries now require the word “PARACETAMOL” in large font on all packaging. In the U.S., proposals are still under review. Until then, you have to be your own advocate.
There’s a new tool in development: smartphone apps that scan barcodes on medicine bottles and calculate your total daily acetaminophen intake. One pilot program in California showed a 40% drop in accidental overdoses among users. It’s not widely available yet-but it’s coming.
What to Do If You Think You’ve Taken Too Much
If you suspect you’ve taken too much acetaminophen-whether it’s 8 pills or 12-don’t wait. Don’t hope it’ll pass. Don’t text a friend. Call Poison Control right now.
In the U.S., dial 1-800-222-1222. In the UK, call 111 or go to 111.nhs.uk. In other countries, find your national poison center number. Tell them exactly what you took, how much, and when. They’ll tell you if you need to go to the hospital.
If you’re in the ER, ask for N-acetylcysteine (NAC). It’s the antidote. It’s not expensive. It’s not experimental. It’s been used for over 40 years. And if given within 8 hours, it works almost every time.
One woman in Bristol took 10 extra-strength Tylenol over 12 hours for back pain. She felt fine until the next morning, when she started vomiting and couldn’t stand up. She called Poison Control. They told her to go to the hospital. She got NAC within 6 hours. Her liver enzymes were high-but they returned to normal in two weeks. No permanent damage.
When Acetaminophen Is Still the Right Choice
Let’s be clear: acetaminophen isn’t the enemy. It’s one of the safest pain relievers when used correctly. For people who can’t take NSAIDs-because of stomach ulcers, high blood pressure, or kidney disease-it’s often the only option.
The American Liver Foundation and the American Association for the Study of Liver Diseases both say: if you have chronic liver disease, you can still use acetaminophen-but at lower doses (under 2,000 mg/day) and only when necessary. Many doctors prefer it over ibuprofen for patients with cirrhosis.
The problem isn’t the drug. It’s the confusion. It’s the assumption that “over-the-counter” means “harmless.” It’s the belief that if you don’t feel sick right away, you’re fine.
Final Rule: When in Doubt, Skip It
If you’re not sure whether a medicine contains acetaminophen, don’t take it. If you’ve already taken some today and you’re considering another, wait. If you’re drinking alcohol, avoid it entirely.
There’s no reward for pushing the limit. No bonus for taking an extra pill because “it’s not working fast enough.” Your liver doesn’t have a reset button. Once it’s damaged, recovery isn’t guaranteed.
Acetaminophen saves lives. But it can end them too. The difference? Awareness. Care. And knowing when to stop.
Can you take acetaminophen every day?
Yes-but only if you stay under 3,000 mg per day and don’t drink alcohol. Long-term daily use, even at low doses, can still cause liver damage over time, especially if you have other risk factors like obesity or hepatitis. If you need pain relief every day, talk to your doctor about alternatives.
Is Tylenol safer than ibuprofen?
It depends. Tylenol (acetaminophen) is easier on the stomach and doesn’t increase bleeding risk like ibuprofen does. But it’s harder on the liver. Ibuprofen can cause kidney problems with long-term use. Neither is “safer” overall-just safer for different people. If you have liver disease, avoid acetaminophen. If you have kidney issues or a history of ulcers, avoid ibuprofen.
How much acetaminophen is toxic for a child?
For children, toxicity starts at 150 mg per kilogram of body weight in a single dose. For a 30 kg (66 lb) child, that’s about 4,500 mg-far more than a typical dose. But children are more sensitive. Always use weight-based dosing, never age-based. Never give adult formulations. Use the measuring tool that comes with the medicine. A teaspoon error can be dangerous.
Can you recover from acetaminophen liver damage?
Yes-if you get treatment early. The liver is one of the few organs that can regenerate. If you receive N-acetylcysteine within 8 hours of overdose, most people recover fully with no lasting damage. If treatment is delayed beyond 24 hours, the risk of permanent damage or death rises sharply. Recovery can take weeks to months, even with treatment.
What are the signs of liver damage from acetaminophen?
Early signs include nausea, vomiting, loss of appetite, and pain under the right ribs. Later signs include yellowing of the skin or eyes (jaundice), dark urine, confusion, swelling in the belly, and extreme fatigue. If you’ve taken acetaminophen and develop any of these, seek help immediately-even if you feel fine.
Does N-acetylcysteine have side effects?
Yes, but they’re mild compared to the risk of liver failure. NAC can cause nausea, vomiting, flushing, or a rash when given intravenously. Oral NAC tastes awful and can cause diarrhea. But these side effects are manageable. The risk of not taking it-especially if you’ve overdosed-is far greater.
Can you take acetaminophen after drinking alcohol?
It’s not recommended. Even one drink can increase your risk. Alcohol slows down how your liver processes acetaminophen, letting more of the toxic byproduct build up. If you’ve had more than two drinks in a day, skip acetaminophen. If you drink regularly, talk to your doctor about safer pain relief options.
Are there alternatives to acetaminophen for pain?
Yes. For mild pain, consider physical therapy, heat packs, or massage. For inflammation-related pain, ibuprofen or naproxen may work-but only if you don’t have stomach, kidney, or heart issues. For chronic pain, talk to your doctor about non-medication options like exercise, cognitive behavioral therapy, or prescription alternatives like duloxetine. Always weigh the risks and benefits.

George Graham
December 4, 2025 AT 13:32I used to take Tylenol like candy after long workdays. Didn't think twice until my buddy ended up in the ER after mixing it with wine. Now I check every label like a hawk. Seriously, if you're on meds, assume acetaminophen is hiding somewhere.
John Filby
December 5, 2025 AT 15:28Just checked my medicine cabinet-turns out my sleep aid has APAP in it. 😳 I’ve been taking that with my headache pills for months. Thanks for the wake-up call. Going to toss the whole stash and start fresh.
Elizabeth Crutchfield
December 5, 2025 AT 22:40omg i had no idea apap was just acetaminophen… i thought it was some fancy new thing. now i feel dumb but also super glad i saw this.
Ben Choy
December 7, 2025 AT 13:15My mum’s got cirrhosis and her doc told her she can have up to 2000mg a day if she’s careful. She writes down every pill like a scientist. I used to tease her… now I do it too. Small habits save lives. 🙌
Emmanuel Peter
December 8, 2025 AT 17:01Why are we acting like this is news? Everyone knows Tylenol kills your liver. The real issue is that people don’t read labels because they’re lazy. Stop blaming the packaging and start taking responsibility. You’re an adult.
Benjamin Sedler
December 8, 2025 AT 21:37Acetaminophen? More like Acetaminophen: The Silent Killer™. Next they’ll tell us water’s dangerous if you drink too much. At this point, I just take ibuprofen and hope my kidneys don’t turn to dust. At least I know what I’m doing.
zac grant
December 10, 2025 AT 08:33As a pharmacist, I see this every week. The real tragedy isn’t the overdose-it’s the delay in seeking help. People wait until Stage 3 because they think, ‘I’m not that sick.’ NAC isn’t magic, but it’s the closest thing we have. Time is liver.
michael booth
December 11, 2025 AT 00:22It is important to note that the human liver possesses a remarkable capacity for regeneration. When acetaminophen toxicity is addressed promptly with N-acetylcysteine, the prognosis is overwhelmingly favorable. Vigilance, not fear, is the appropriate response.
Carolyn Ford
December 11, 2025 AT 21:00Ugh. Another ‘awareness’ post. You know what’s worse than acetaminophen? People who think they’re ‘helping’ by scaring everyone into panic. I’ve taken Tylenol daily for 15 years. I drink wine. I’m fine. Your fearmongering won’t make me feel guilty.
Alex Piddington
December 13, 2025 AT 13:51My kid’s pediatrician gave us a printed chart with weight-based dosing. We keep it taped to the fridge. I also scan every bottle with the app they mentioned. It’s not paranoia-it’s parenting. And yes, I still use the syringe. No spoons. Ever.
Libby Rees
December 15, 2025 AT 02:22My grandmother died from liver failure after taking cold medicine for a week. She didn’t know it had acetaminophen. I now check every label before I buy anything. Simple. Necessary.
Ollie Newland
December 15, 2025 AT 09:27My liver enzymes were through the roof last year. Turns out I was taking Vicodin for back pain + extra Tylenol for migraines. Didn’t realize they were the same drug. Got NAC in time. Now I’m off everything but physical therapy. Liver’s back to normal. Don’t be me.