Acromegaly Surgery: How It Fits Into Modern Treatment
 Oct, 12 2025
Oct, 12 2025
Acromegaly Surgery Success Calculator
Surgical Success Rate Calculator
Estimate the potential success rate for acromegaly surgery based on tumor type.
Estimated Success Rate
Note: Success rates are based on published data from major medical centers.
Microadenomas typically have a 70-80% remission rate, while macroadenomas have a 50-60% rate.
When a patient is diagnosed with Acromegaly is a chronic condition caused by excess growth hormone, usually from a pituitary adenoma, the treatment plan often starts with a discussion about surgery. Doctors weigh the size of the tumor, hormone levels, and the patient’s overall health before deciding whether to operate, medicate, or combine approaches.
Why Surgery Is Considered First‑Line
In most guidelines published after 2020, surgical removal of the adenoma remains the preferred initial step for patients whose tumors are accessible and who have no contraindications. The main goal is to eliminate the source of excess growth hormone (GH) and thereby normalize insulin‑like growth factor‑1 (IGF‑1) levels.
Transsphenoidal surgery is a minimally invasive technique that reaches the pituitary through the nose and sphenoid sinus offers a high remission rate-around 70‑80% for microadenomas and 50‑60% for macroadenomas when performed by experienced teams.
Choosing the Right Surgical Approach
The two most common routes are:
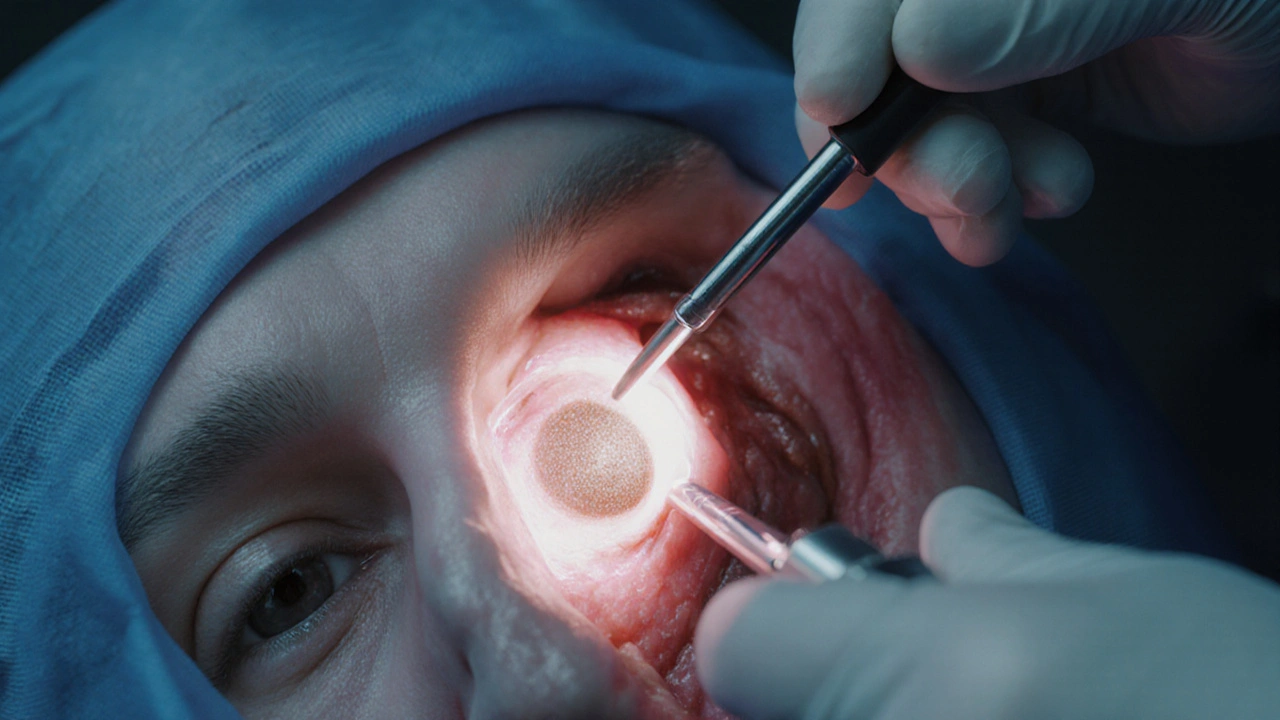
- Endoscopic transsphenoidal: Uses a camera and LED light, giving the surgeon a panoramic view of the tumor.
- Microscopic transsphenoidal: Relies on a traditional operating microscope; still used in some centres where endoscopic gear is unavailable.
Endoscopic methods have become the standard in the UK and many European centres because they reduce nasal trauma and shorten recovery.
What Happens Before the Operation
Preparation begins with a high‑resolution MRI scan of the sellar region to map the tumor’s dimensions and its relationship to the cavernous sinus. Hormone panels measuring GH and IGF‑1 are repeated to confirm active disease. Endocrinologists may start short‑acting somatostatin analogs a few days before surgery to stabilize hormone spikes and lower the risk of intra‑operative cardiovascular events.
Inside the Operating Room
Under general anesthesia, the surgeon inserts a thin endoscope through one nostril. Real‑time navigation systems linked to the pre‑op MRI guide the instrument to the tumor. The adenoma is gently peeled away from the normal pituitary tissue, aiming to preserve as much healthy gland as possible.
Key technical points that influence success include:
- Complete removal of the visible tumor capsule.
- Adequate decompression of the surrounding cavernous sinus.
- Minimal manipulation of the normal pituitary to avoid post‑op hypopituitarism.
Recovery and Early Outcomes
Most patients spend one night in a surgical ward and are discharged within 2-3days. Nasal packing is rarely needed with endoscopic tools, which means less discomfort. Hormone levels are checked on day1 and again at 6weeks. A drop in GH to below 1µg/L after an oral glucose tolerance test usually signals remission.
Possible early complications include:
- Transient diabetes insipidus (about 10% of cases).
- CSF leak, often repaired intra‑operatively but may require a lumbar drain.
- Nasal crusting and mild sinusitis, treatable with saline sprays.
Long‑Term Success Rates
Data from the European Society of Endocrinology’s 2023 registry show that 5‑year disease‑free survival reaches 65% for microadenomas and 45% for macroadenomas after a single operation. Patients who achieve biochemical remission enjoy lower mortality, reduced cardiovascular risk, and a reversal of soft‑tissue overgrowth.
When Surgery Alone Isn’t Enough
Residual tumor or persistent hormone elevation may call for adjunct therapies:
- Somatostatin analogs such as octreotide or lanreotide, bind to receptors on tumor cells to curb GH secretion.
- GH receptor antagonists like pegvisomant block the action of IGF‑1 on peripheral tissues.
- Fractionated stereotactic radiotherapy targets leftover tissue, offering a delayed but durable control.
Combination therapy often yields the highest chance of normalizing IGF‑1 when surgery falls short.
How to Decide: A Simple Comparison
| Approach | Primary Goal | Typical Success Rate | Key Advantages | Main Drawbacks |
|---|---|---|---|---|
| Transsphenoidal Surgery | Remove adenoma source | 70‑80% (micro) / 50‑60% (macro) | Rapid hormone control; potential cure | Operative risk; possible hypopituitarism |
| Somatostatin Analogs | Suppress GH secretion | 45‑60% biochemical control | Non‑invasive; can shrink tumor | Long‑term injections; variable response |
| GH Receptor Antagonist | Block IGF‑1 effects | 40‑55% IGF‑1 normalization | Effective when GH remains high post‑surgery | Daily subcutaneous dosing; expensive |
| Fractionated Radiotherapy | Destroy residual cells | ≈70% long‑term control | Useful for refractory cases | Delayed effect (3‑5years); risk of hypopituitarism |

Practical Tips for Patients Considering Surgery
- Choose a centre that performs at least 20 pituitary surgeries a year; volume correlates with better outcomes.
- Ask about the surgeon’s experience with endoscopic techniques.
- Discuss pre‑operative medical therapy; short‑acting analogs can lower intra‑operative GH spikes.
- Plan for a brief period of endocrine follow‑up-blood tests at 6weeks, 3months, and then annually.
- Be aware of signs of CSF leak (clear nasal drainage) and seek prompt care.
Future Directions in Acromegaly Surgery
Robotic assistance and augmented‑reality overlays are being trialled in a handful of UK neurosurgical units. Early data suggest improved visualization of cavernous sinus invasion, which could raise remission rates for large macroadenomas. Genetic profiling of adenomas may also steer surgeons toward more aggressive resection when certain mutation patterns predict rapid growth.
While these innovations are promising, the core principle remains unchanged: removing the tumor source is the fastest way to halt the harmful cascade of excess growth hormone.
Key Takeaways
- Surgery, especially endoscopic transsphenoidal, is the first‑line treatment for most operable acromegaly cases.
- Success rates depend on tumor size; microadenomas respond best.
- Post‑operative hormone monitoring guides the need for additional medical or radiotherapy.
- Choosing an experienced pituitary centre dramatically improves outcomes.
- Emerging technologies aim to boost remission for larger tumors, but the surgical goal stays the same.
Frequently Asked Questions
Can acromegaly be cured without surgery?
Medical therapy alone can control hormone levels in many patients, but true cure-meaning the tumor disappears and hormone production normalizes permanently-is rare without removing the adenoma. Most specialists recommend surgery first, then add medication if needed.
What are the risks of transsphenoidal surgery?
The most common issues are temporary diabetes insipidus, mild CSF leaks, and nasal discomfort. Permanent hormone deficiencies occur in about 5‑10% of cases, and serious complications such as major bleeding are uncommon in high‑volume centres.
How long does it take to see hormone improvement after surgery?
GH levels usually drop within 24hours, while IGF‑1 may take 2‑4weeks to normalize. Follow‑up labs at 6weeks and 3months are standard to confirm remission.
Is there an age limit for surgery?
Chronologically older adults can undergo surgery if they are fit for general anaesthesia. The decision hinges on overall health, not age alone. Frail patients may be steered toward medical management.
Will I need lifelong medication after a successful operation?
If hormone levels stay normal for at least a year post‑op, many patients stop medication entirely. However, some may develop recurrent disease and require intermittent drugs.

Jim Butler
October 12, 2025 AT 18:01Great overview of acromegaly surgery! It really highlights how endoscopic techniques have become the norm, and the success rates are encouraging 😊👍
Renee van Baar
October 14, 2025 AT 11:41The step‑by‑step breakdown makes it easy to grasp what patients can expect before and after the operation. I especially appreciate the practical tips about choosing a high‑volume centre. Those details can make a huge difference in outcomes.
Mithun Paul
October 16, 2025 AT 05:21While the article is thorough, it glosses over the variability in remission rates across different surgical teams. The cited data from the European Society of Endocrinology does not account for case mix bias. Moreover, the discussion of adjunct therapies could benefit from a more critical appraisal of cost‑effectiveness.
Sandy Martin
October 17, 2025 AT 23:01The postoperative hormone monitoring schedule described here is spot on for most centres.
However, many patients forget that the glucose tolerance test must be performed after an overnight fast.
In practice, the GH nadir often drops below 1 µg/L within 24 hours, but IGF‑1 can linger for weeks.
It is crucial to schedule that first IGF‑1 check at the six‑week mark, otherwise false‑positives may arise.
Some surgeons also recommend a baseline cortisol level to rule out adrenal insufficiency before dischargee.
A common oversight is neglecting to assess sodium levels, especially if the patient received intra‑operative desmopressin.
Patients with macroadenomas should be warned that delayed remission is possible, and a second MRI at 6 months can reveal residual tissue.
The article mentions CSF leak rates but does not emphasise that endoscopic skull‑base reconstruction has reduced that risk dramatically.
I've seen cases where a simple fat graft and fibrin sealant prevented the need for a lumbar drain.
Another point worth noting is that transient diabetes insipidus usually resolves within a week, yet many clinicians prescribe thiazide diuretics too early.
The authors' suggestion to use short‑acting somatostatin analogs pre‑op is sound, but insurance barriers can delay therapy.
In low‑resource settings, some teams opt for a staged surgery combined with radiotherapy, which can lower overall morbidity.
Long‑term follow‑up should also include bone density scans, as untreated acromegaly can lead to osteoporosis.
Finally, patient education about the signs of CSF leak-clear, watery nasal discharge-cannot be over‑stated.
By integrating these practical nuances into the care pathway, outcomes can be further optimised.
Steve Smilie
October 19, 2025 AT 16:41One cannot ignore the burgeoning renaissance of robotic assistance in pituitary surgery; it heralds an epoch where precision melds with artistry. The burgeoning palettes of augmented‑reality overlays will soon render the cavernous sinus a translucent tapestry, allowing surgeons to excise macroadenomas with Da Vinci‑like grace. Such innovations, albeit nascent, promise to catapult remission rates beyond the current ceiling.
Josie McManus
October 21, 2025 AT 10:21That sounds amazing, but let’s keep it real-most hospitals still lack the budget for those fancy rigs. Until the tech becomes commonplace, patients will continue to rely on the tried‑and‑true endoscopic approach.
Heather Kennedy
October 23, 2025 AT 04:01From a neuro‑endocrine standpoint, the intra‑operative navigation systems referenced are based on fused MRI‑CT datasets, which improve tumor delineation by up to 15 %. Additionally, employing intra‑operative frozen sections can confirm complete adenoma removal, reducing the need for subsequent radiotherapy.
Janice Rodrigiez
October 24, 2025 AT 21:41Bottom line: surgery still beats meds for a cure.
Roger Cardoso
October 26, 2025 AT 14:21All that high‑tech fluff just distracts from the fact that surgical skill, not gadgets, determines outcomes. The data you cite are from elite centers, not the average hospital.
barry conpoes
October 28, 2025 AT 08:01Our nation's health system should prioritize funding for pituitary surgery programs because acromegaly patients are losing valuable productivity due to untreated disease.
Kristen Holcomb
October 30, 2025 AT 01:41Absolutely, investing in experienced pituitary teams will cut long‑term healthcare costs and improve quality of life for countless Americans.
justin davis
October 31, 2025 AT 19:21Wow, another groundbreaking revelation-if you cut the tumor, hormones go down. Who would’ve thought?!
David Lance Saxon Jr.
November 2, 2025 AT 13:01The surgical excision of a pituitary adenoma is, in essence, a tangible manifestation of humanity's quest to restore homeostasis amidst chaotic endocrine flux. It underscores the dialectic between invasive intervention and the body's intrinsic regulatory mechanisms. When we wield scalpel and endoscope, we are not merely removing tissue; we are redefining the ontological parameters of growth. This interplay invites a deeper contemplation of what it means to cure versus merely manage a condition.