Addressing Health Disparities in Medication Safety Research: Why Equity Can't Wait
 Jan, 17 2026
Jan, 17 2026
Medication Safety Disparity Calculator
Calculate Your Risk
Medication errors don’t affect everyone equally
Every year, millions of people around the world experience preventable harm from medications. Some get the wrong dose. Others take drugs that interact badly. Some never get the right medicine at all. But here’s the truth no one talks about enough: these mistakes don’t happen by chance. They cluster around the same groups of people who already face the biggest barriers in healthcare-Black, Hispanic, Indigenous, elderly, non-English speakers, and low-income communities.
The World Health Organization calls this medication safety a global crisis. In 2017, they launched the ‘Medication Without Harm’ initiative to cut severe, avoidable harm by 50% in five years. The cost of these errors? $42 billion a year. But behind that number are real people-grandparents who don’t understand their pill bottles, single mothers skipping doses because they can’t afford them, immigrants who can’t explain their symptoms to a doctor who doesn’t speak their language.
Why are some patients invisible in safety data?
In 2021, researchers in the UK reviewed over 12,000 medication incident reports across five NHS hospitals. What they found was shocking: patients from white and Black ethnic groups had far more reports filed than those from South Asian, Chinese, or other minority backgrounds. Not because they made more mistakes. Because their concerns were ignored.
Language isn’t the only barrier. Cultural distrust runs deep. A study of African American public health students in Georgia showed how clinicians often dismissed patient concerns based on unconscious bias. One patient said, “I told them my chest hurt. They said it was anxiety. I had a heart attack two days later.” That’s not an outlier. It’s a pattern.
When patients don’t feel heard, they stop speaking up. And when they stop speaking up, their errors disappear from the data. That means hospitals think they’re doing fine-when they’re actually missing the most dangerous cases.
Clinical trials leave people behind
New drugs are tested in clinical trials. But who gets to be in those trials? Not enough people of color. A Kaiser Family Foundation analysis of FDA-approved drugs from 2014 to 2021 found that Black participants made up only one-third of what their disease burden would suggest. In other words, if Black people were getting cancer at twice the rate of white people, you’d expect them to be half the trial population. They weren’t even close.
That has deadly consequences. In 2021, the U.S. Preventive Services Task Force couldn’t issue specific colorectal cancer screening guidelines for Black Americans-even though they have the highest death rates-because there wasn’t enough data from studies that included them. How do you protect someone when you don’t even know how the medicine affects them?
And when new drugs finally come out? They’re expensive. In 2022, nearly 19% of Hispanic Americans and 11.5% of Black Americans were uninsured. Compare that to 7.4% of white Americans. So even if a safer drug exists, it’s out of reach for the people who need it most.
Doctors don’t always see the problem
Implicit bias isn’t just a buzzword. It’s a clinical risk. A 2024 study in JAMA Network Open found three major drivers of unsafe medication use in marginalized communities: lack of access to care, biased prescribing habits, and people turning to unsafe over-the-counter alternatives because they can’t get proper prescriptions.
One of the most damaging myths? That Black patients feel less pain. For decades, doctors believed this-and prescribed less pain relief accordingly. That myth still lingers. A patient with sickle cell disease in Texas told researchers she was called “drug-seeking” six times before being given opioids for a crisis. She ended up in the ER with organ failure.
Technology isn’t always the answer either. Artificial intelligence tools used to predict which patients are at risk for medication errors have been shown to mislabel Black patients as lower risk, simply because they’ve historically had less access to care. The algorithm sees less data and assumes less need. It’s not smarter. It’s just biased.
What’s being done-and what’s not
The Joint Commission now lists equity as a formal patient safety goal. That’s progress. The WHO’s ‘Medication Without Harm’ framework includes equity as a core pillar. But here’s the gap: only 32% of U.S. hospitals have any formal program to tackle medication safety disparities-even though 78% say it’s a priority.
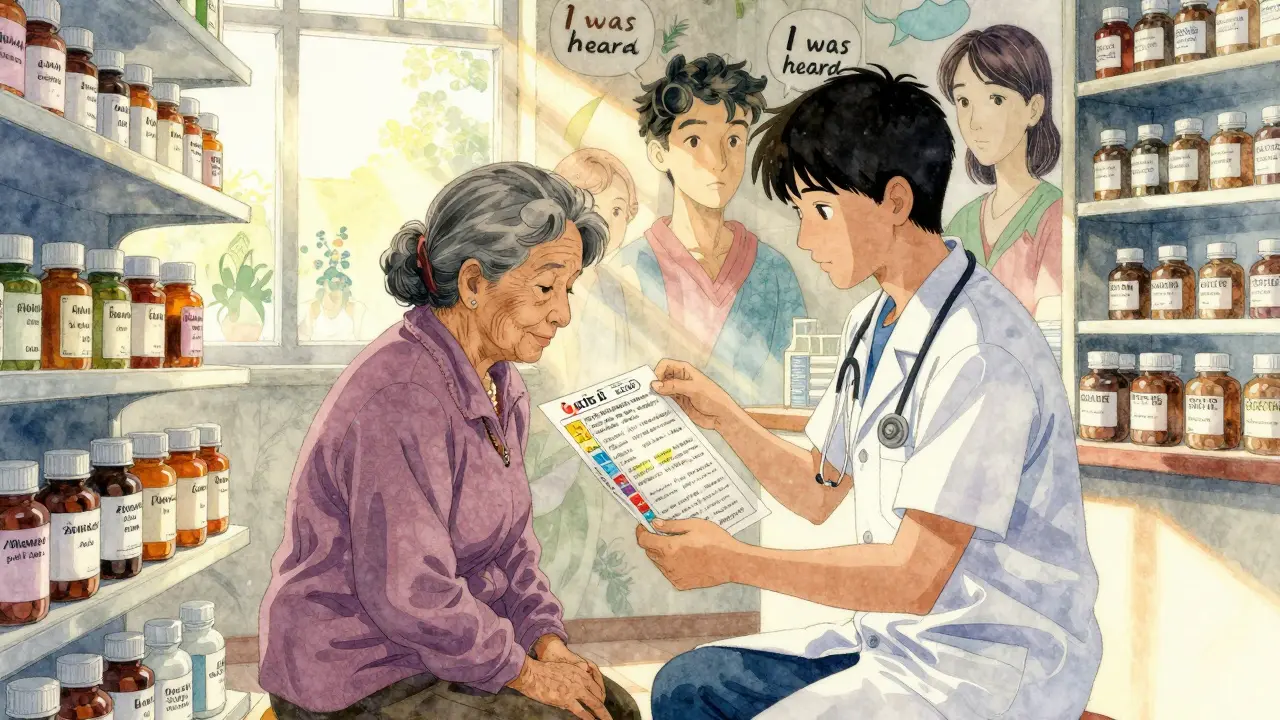
Why? Because fixing this isn’t about buying new software. It’s about changing culture. It’s about hiring bilingual staff. Training clinicians to recognize their own biases. Creating feedback loops where patients from marginalized communities help design safety protocols-not just sit through them.
Some hospitals in Boston and Chicago are trying. They’ve embedded community health workers into pharmacy teams. They’ve translated medication instructions into 12 languages. They’ve started listening sessions where patients bring their pill bottles and say, “This doesn’t make sense.” And guess what? The number of medication errors dropped by 40% in two years.
The fix isn’t complicated. It’s just hard.
You don’t need a billion-dollar tech platform to fix this. You need:
- Language services that actually work-not just a phone line that never connects
- Standardized reporting tools that track patient demographics so disparities show up in the data
- Clinical training that includes real stories from patients, not just PowerPoint slides
- Drug pricing policies that don’t leave 1 in 5 Black or Hispanic families choosing between insulin and rent
- Community advisory boards that have real power to change hospital policies
The biggest myth? That this is a social issue, not a medical one. But the Agency for Healthcare Research and Quality says it plainly: equity is patient safety. When a person can’t get their medicine because of their race, language, or income, it’s not a failure of policy. It’s a failure of care.
And that failure kills.
What happens if we don’t act?
If nothing changes, the gap will widen. By 2030, the global patient safety market is expected to hit $12.4 billion. But if that money goes only into flashy dashboards and automated alerts, while real people still struggle to be heard, we’re not improving safety-we’re just automating inequality.
Imagine a world where every patient, no matter their background, gets the same chance to be safe. Where a Black grandmother in Detroit, a Spanish-speaking elder in Phoenix, and a low-income teen in Bristol all get the same clear instructions, the same respectful care, and the same access to life-saving drugs.
That world is possible. But it won’t happen by accident. It will take intentional action. Real listening. And the courage to admit that our systems have been broken for a long time.
The data is clear. The solutions exist. What’s missing is the will.

Lydia H.
January 17, 2026 AT 20:24It’s not about tech. It’s about showing up.
Astha Jain
January 18, 2026 AT 00:53Erwin Kodiat
January 18, 2026 AT 23:42We started drawing pictures. No more jargon. Errors dropped 40%. It’s not rocket science. It’s respect.
Jacob Hill
January 19, 2026 AT 03:20Lewis Yeaple
January 20, 2026 AT 15:05Jake Rudin
January 21, 2026 AT 12:00Equity isn’t a feature. It’s a rewrite.
Josh Kenna
January 22, 2026 AT 20:20Valerie DeLoach
January 22, 2026 AT 23:09Christi Steinbeck
January 23, 2026 AT 19:14Jackson Doughart
January 23, 2026 AT 21:47Malikah Rajap
January 25, 2026 AT 00:37sujit paul
January 25, 2026 AT 03:39Tracy Howard
January 27, 2026 AT 02:14