Alcohol and Diabetes Medications: How to Avoid Dangerous Low Blood Sugar
 Dec, 16 2025
Dec, 16 2025
When you have diabetes and take medication to control your blood sugar, drinking alcohol isn’t just about moderation-it’s about survival. A single drink can send your blood sugar crashing, even hours later, and you might not even realize it’s happening. This isn’t theoretical. It’s a real, life-threatening interaction that happens every day to people who think they’re being careful.
Why Alcohol and Diabetes Medications Don’t Mix
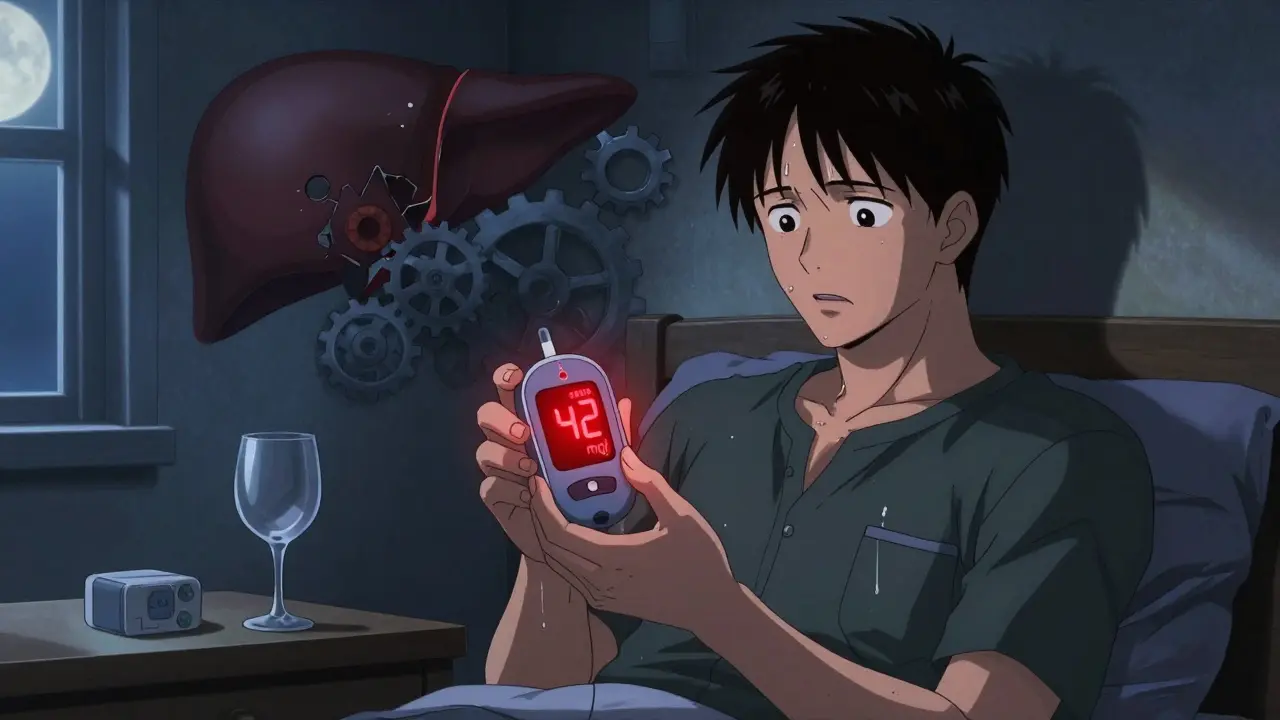
Your liver has one job when you’re fasting: keep your blood sugar steady by releasing stored glucose. Alcohol throws a wrench in that system. It doesn’t just lower your blood sugar-it blocks your liver from making more. That’s fine if you’re not on diabetes meds. But if you’re taking insulin, sulfonylureas like glipizide or glyburide, or even metformin, alcohol turns a manageable situation into a medical emergency. The problem isn’t just the alcohol itself. It’s how it interacts with your medication. Sulfonylureas force your pancreas to pump out more insulin. Alcohol shuts down your liver’s ability to fight back. The result? Blood sugar plummets. A 2020 meta-analysis found that combining alcohol with sulfonylureas increases hypoglycemia risk by more than two times. With insulin? The danger lasts up to 24 hours. You could go to bed feeling fine, wake up confused, and find your glucose at 42 mg/dL.Metformin and Alcohol: The Silent Lactic Acidosis Risk
Metformin is one of the most common diabetes drugs. Many assume it’s safe with alcohol because it doesn’t cause low blood sugar on its own. That’s misleading. The FDA requires a boxed warning on metformin labels for a reason: alcohol raises your risk of lactic acidosis-a rare but deadly buildup of acid in the blood. A 2022 JAMA study showed this risk jumps 5.7 times when you drink while on metformin. Symptoms don’t always look like typical low blood sugar. Instead of sweating or shakiness, you might feel dizzy, nauseous, or have muscle pain so severe it feels like you’ve been running marathons. Your heart races. Your breathing gets shallow. These signs are often mistaken for being drunk. If you’re out with friends and pass out, no one will know it’s not just intoxication. They won’t know to check your blood sugar. They won’t know to call 911.What Counts as a ‘Safe’ Drink?
There’s no such thing as a completely safe drink if you’re on diabetes medication. But there are safer choices. The American Diabetes Association’s 2023 guidelines say: one drink per day for women, two for men. But that’s only if you follow the rules. A standard drink means:- 12 oz of light beer (under 5g carbs)
- 5 oz of dry wine (under 1g sugar)
- 1.5 oz of distilled spirits (vodka, gin, whiskey) mixed with soda water or diet tonic

The Hidden Danger: Nighttime Hypoglycemia
Most people think the risk ends after a few hours. It doesn’t. Alcohol delays your liver’s glucose production for up to 24 hours. That’s why 82% of alcohol-related hypoglycemic emergencies happen between 11 PM and 6 AM, according to research from USC’s Clinical Diabetes Programs. You might have eaten dinner. You might have checked your blood sugar before bed and it was 110 mg/dL. You think you’re fine. But your liver is still busy processing alcohol. By 3 AM, it’s out of glucose to release. Your insulin is still working. Your blood sugar drops. You don’t wake up. You don’t feel the warning signs. Your body’s natural defenses-epinephrine, glucagon-are suppressed by alcohol. A 2021 study found epinephrine response drops by 42% after drinking. This isn’t just a theory. On diabetes forums, users describe waking up in the ER after needing glucagon injections. One man, on insulin pump therapy, had three hypoglycemic episodes after just two beers. He didn’t realize the danger would hit hours later while he slept.How to Drink Safely (If You Choose To)
If you decide to drink, treat it like a medical procedure. Follow these steps:- Never drink on an empty stomach. Always eat food with carbohydrates-like whole grain bread, rice, or fruit-before and while drinking.
- Check your blood sugar before you start. If it’s below 100 mg/dL, don’t drink. Wait and eat something.
- Check it again 2 hours after your last drink. If it’s below 100 mg/dL, eat 15-30 grams of fast-acting carbs: 4 oz of fruit juice, 3-4 glucose tablets, or 1 tablespoon of honey.
- Check it before bed. If it’s below 100 mg/dL, eat a small snack with protein and complex carbs: peanut butter on whole wheat, a hard-boiled egg with an apple.
- Wear medical ID. A bracelet or necklace that says ‘Diabetic’ could save your life if you’re found unconscious.
- Tell someone. Make sure a friend or family member knows you have diabetes and what to do if you seem confused, sweaty, or unresponsive.
What Not to Do
Don’t assume low-carb drinks are safe. Sugar-free mixers still let alcohol do its damage. Don’t skip meals to ‘save carbs’ for later. That’s a recipe for disaster. Don’t rely on how you feel. Alcohol masks hypoglycemia symptoms. You might feel fine-even dizzy or tired-but your blood sugar could be tanking. And don’t believe the myth that ‘I don’t have hypoglycemia often, so I’m fine.’ People who rarely have lows are the most vulnerable. Their bodies don’t trigger warning signs anymore. Alcohol makes that worse.
What the Experts Say
Dr. Robert Gabbay, Chief Scientific Officer of the American Diabetes Association, puts it bluntly: “A mojito on an empty stomach at happy hour is significantly riskier than a glass of wine with dinner.” The Endocrine Society warns against chlorpropamide-a sulfonylurea that can cause flushing, nausea, and heart palpitations when mixed with alcohol. It’s rarely prescribed now, but if you’re on it, avoid alcohol entirely. Kaiser Permanente’s 2023 patient safety report found that 38% of patients who had alcohol-related hypoglycemia didn’t recognize the symptoms because alcohol impaired their thinking. They thought they were just drunk. They didn’t test their blood sugar. They didn’t get help. They passed out.Emerging Solutions
New tech is helping. Dexcom’s G7 continuous glucose monitor, released in late 2023, now lets you log alcohol intake. The app then predicts hypoglycemia risk over the next 24 hours and sends alerts. Early data shows it reduces nighttime lows by nearly a third. A 2024 pilot study found that drinking alcohol within 4 hours after dinner-instead of late at night-cut nocturnal hypoglycemia by 31%. Timing matters. Eating and drinking together helps your liver stay balanced. Future research is looking at genetics. Some people have a version of the CYP2E1 enzyme that breaks down alcohol slower, making them more prone to dangerous interactions. This could one day lead to personalized advice based on DNA.Final Reality Check
You don’t have to quit alcohol forever. But you have to treat it like a medication-with rules, timing, and consequences. If you’re on insulin or sulfonylureas, every drink carries risk. If you’re on metformin, every drink carries a different kind of risk. If you’re unsure, ask your doctor. Don’t guess. Don’t rely on internet advice. Don’t assume you’re fine because you’ve had a drink before. Your body is already working hard to keep you alive. Don’t make it fight alcohol on top of that.Alcohol and diabetes medications don’t just interact-they collide. And the fallout is often silent, deadly, and preventable.

Jonathan Morris
December 16, 2025 AT 21:37Let me break this down with peer-reviewed data: alcohol inhibits gluconeogenesis via NADH accumulation in hepatocytes, which shifts the lactate-pyruvate ratio and suppresses hepatic glucose output. Sulfonylureas exacerbate this by forcing insulin secretion regardless of glycemic status. The 2.1x increased hypoglycemia risk (95% CI: 1.8–2.4) from the 2020 meta-analysis is statistically significant, p < 0.001. The FDA’s boxed warning on metformin isn’t hyperbole-it’s a pharmacokinetic inevitability. Lactic acidosis mortality is 30–50%. You’re not ‘being careful’ if you’re drinking after 8 PM. Your liver isn’t a switch-it’s a slow, poisoned engine.
Also, the Dexcom G7 algorithm? It’s trained on 12,000 patient-days. It doesn’t guess. It calculates. If your app isn’t logging alcohol, you’re flying blind. And no, ‘I only have one drink’ doesn’t matter. Half-life of ethanol is 4–5 hours. Gluconeogenesis suppression lasts 18–24. You’re not in control. Your biochemistry is.
Stop romanticizing ‘moderation.’ This isn’t wine tasting. It’s a metabolic landmine.
Donna Packard
December 17, 2025 AT 09:14I know how scary this sounds. I’ve been on insulin for 12 years, and I used to think a glass of wine was fine. Then I woke up at 3 a.m. with a glucose of 38, shaking, confused, and my husband had no idea why I was like that. I didn’t even know I was low until I saw the number.
I don’t drink anymore. Not because I’m giving up, but because I love my life too much to risk it. The rules in this post? I follow them all-even the one about telling someone. My husband knows what to do now. And honestly? That peace of mind is worth more than any drink.
You’re not alone. We’re all trying to live well with this. Be gentle with yourself.
Patrick A. Ck. Trip
December 18, 2025 AT 06:14While i must say this article is very well researched and presents a compelling case, i must note that i have personally consumed alcohol while on metformin for over 15 years without incident. Perhaps individual metabolic variation plays a larger role than the generalized warnings suggest. I do not consume alcohol on an empty stomach, and i always monitor my glucose levels before and after. I believe that blanket statements may inadvertently discourage patients from engaging in social activities that contribute to mental well-being.
That said, i do appreciate the cautionary tone and the emphasis on medical ID and communication with others. These are vital practices regardless of one’s personal risk profile. Perhaps the future of diabetes management lies in personalized risk modeling rather than one-size-fits-all guidelines.
Thank you for the thoughtful piece. I hope it encourages more nuanced conversations rather than fear-based avoidance.
Virginia Seitz
December 18, 2025 AT 18:45Just say no to mojitos 😅
One beer? Maybe. But sugar = bad. Liver = tired. Sleep = risky.
Check your sugar. Tell someone. Wear your ID. That’s it. 💙
Peter Ronai
December 19, 2025 AT 22:58Oh here we go. Another fear-mongering article from the ADA’s PR department. ‘One drink can kill you’? Please. I’ve had 3 beers after dinner on insulin for 8 years and never had a problem. My A1c is 5.8. My glucose monitor shows no crashes. You’re scaring people into thinking they can’t live normal lives.
And what’s this ‘lactic acidosis’ nonsense? Metformin and alcohol? That’s a 0.01% risk for healthy people. You’re acting like we’re all walking time bombs. I’ve seen more people die from heart disease because they quit wine and got depressed than from alcohol-induced hypoglycemia.
Stop infantilizing diabetics. We’re not children. We can make our own choices. If you want to live like a monk, fine. But don’t make the rest of us feel guilty for enjoying a drink with friends.
Also-Dexcom G7? That’s a $1,200 device. Not everyone can afford it. Your ‘solutions’ are for the rich. The rest of us are just trying to survive.
Steven Lavoie
December 20, 2025 AT 06:31I appreciate the depth of this piece. The data is clear, the risks are real, and the advice is practical. I’ve worked in endocrinology for 18 years, and I’ve seen too many patients come in after midnight with glucose levels in the 20s-unconscious, no one knowing why.
One thing I’d add: it’s not just about the drink. It’s about the context. Drinking alone at night? High risk. Drinking with friends after dinner, with food, with someone who knows your condition? Much lower risk. The difference isn’t the alcohol-it’s the safety net.
And to those who say ‘I’ve never had a problem’-you’re lucky. Not immune. Hypoglycemia doesn’t always announce itself. Sometimes, it just… happens. And then it’s too late.
This isn’t about shame. It’s about awareness. And awareness saves lives.
Jane Wei
December 20, 2025 AT 08:15Man, I used to think I was fine with a beer after work. Then I passed out on the couch last winter. Woke up in the ER. They said my sugar was 29. I didn’t even feel like I was low-just tired. Turns out alcohol made my body ignore all the warning signs.
Now I drink soda water with lime. Still feel like I’m at the bar. Still hang out with friends. Just… no alcohol.
Worth it.
Jody Patrick
December 20, 2025 AT 20:43America’s getting soft. Back in my day, people drank and handled their business. You want to drink? Fine. But don’t blame the medicine. Blame your own weakness. If you can’t handle a drink, don’t take the meds. Simple.
Radhika M
December 20, 2025 AT 22:30As a nurse in Mumbai, I see many patients with diabetes who drink because they think ‘it’s just one glass.’ I tell them: your liver is like a phone battery. Alcohol is like a virus draining it while you sleep. You don’t see it, but it’s dying.
Don’t wait for emergency. Check sugar. Eat before. Tell someone. Wear ID. It’s simple. And it saves lives.
God bless you all.