Allergy and Cold Medications: How to Avoid Dangerous Drug Interactions
 Feb, 10 2026
Feb, 10 2026
Medication Interaction Checker
This tool helps you identify potentially dangerous interactions between cold/flu medications and other drugs you're taking. Always consult your doctor or pharmacist before combining medications.
Results
Every winter, millions of people reach for combination cold and allergy meds thinking they’re making things easier. One pill for a runny nose, another for a cough, and maybe a third for a headache. But here’s the truth: combination medications are convenient - and dangerously misleading.
You might not realize it, but the bottle in your medicine cabinet could be quietly stacking up risks you didn’t sign up for. Acetaminophen in your cold tablet? Same as the one in your pain reliever. Phenylephrine in your nasal spray? That’s the same ingredient in your allergy pill. And if you’re on an antidepressant? You could be walking into a medical emergency without even knowing it.
What’s Really in Your Combination Cold and Allergy Medicine?
Most over-the-counter (OTC) cold and allergy products don’t just contain one active ingredient. They pack in two, three, or even four. That’s the whole point - to treat multiple symptoms at once. But that convenience hides a hidden cost: overlap.
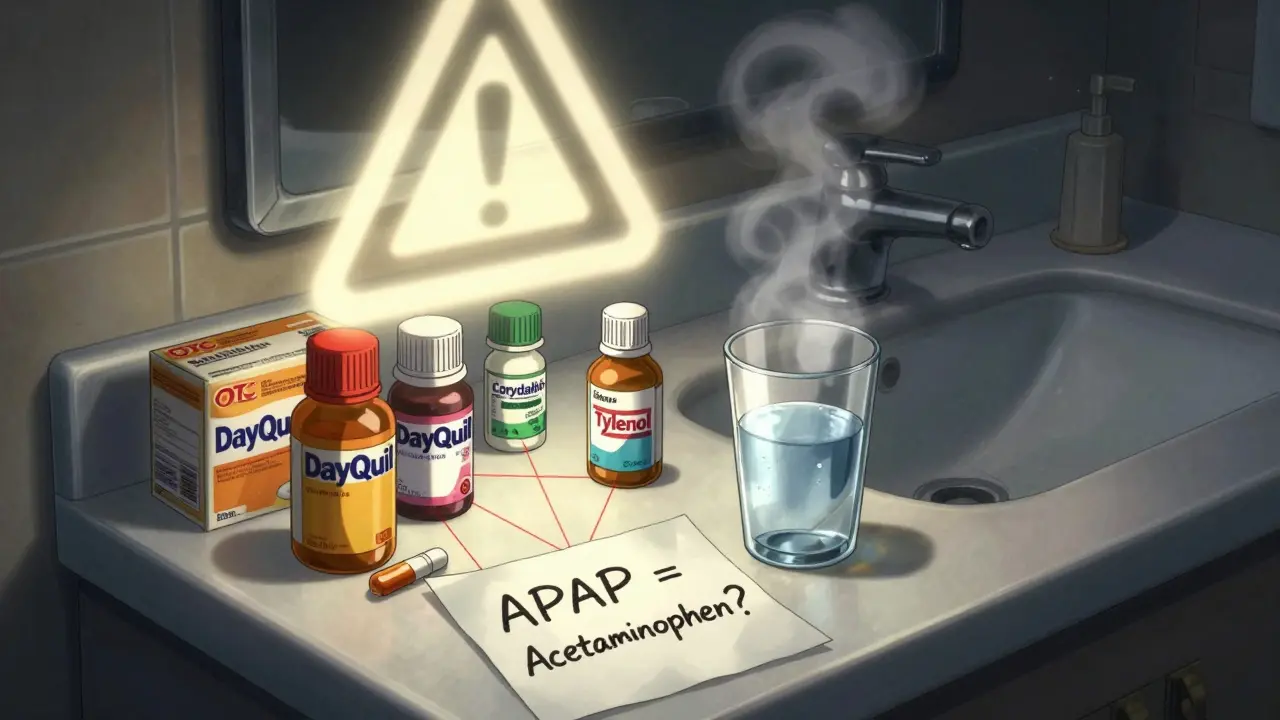
Take DayQuil, Tylenol Sinus, or Coricidin HBP. Look at the label. You’ll likely see:
- Acetaminophen (APAP) - for pain and fever
- Pseudoephedrine or Phenylephrine - for nasal congestion
- Dextromethorphan (DM) - for cough suppression
- Chlorpheniramine or Diphenhydramine - for runny nose and sneezing
Each of these has its own risks. Acetaminophen can cause liver damage if you take more than 4,000mg in a day. But here’s the kicker: many people don’t realize they’re already hitting that limit because they’re taking Tylenol for a headache on top of their cold medicine.
According to CDC data, around 6.7 million Americans accidentally overdose on acetaminophen every year - mostly because they didn’t check the label. And that’s just one ingredient.
The Hidden Interaction: Acetaminophen + Phenylephrine
You’ve probably heard that phenylephrine doesn’t work well as a decongestant. A 2022 study from the University of Florida and Rutgers found that 10mg of oral phenylephrine - the dose in most OTC products - is no better than a placebo. But here’s what nobody’s talking about: when you combine it with acetaminophen, something strange happens.
Research published in the Journal of Clinical Pharmacology in 2014 showed that acetaminophen increases phenylephrine’s absorption by four times. That means the little bit of decongestant in your cold tablet suddenly becomes much stronger in your bloodstream.
The result? Higher risk of high blood pressure, dizziness, rapid heartbeat, and tremors. New Zealand research cited in HealthDay News found phenylephrine-acetaminophen combos had 4.1 times higher risk of hypertension-related side effects than acetaminophen alone.
And yet, these combinations are still on shelves everywhere. Why? Because the FDA still considers them “generally recognized as safe and effective” - even if the decongestant part doesn’t actually work. The agency’s hands are tied by old rules from the 1980s. A 2023 advisory committee meeting is reviewing whether phenylephrine should be removed from OTC products entirely.
Pseudoephedrine vs. Phenylephrine: Which Is Safer?
If you’re looking for real decongestant power, pseudoephedrine (found in Sudafed) is still the gold standard. Studies show it reduces nasal congestion by 65%, compared to just 45% with phenylephrine.
But it comes with trade-offs. Pseudoephedrine raises systolic blood pressure by 8-12mmHg and increases heart rate by 5-8 beats per minute. That’s why it’s kept behind the pharmacy counter in the U.S. - you have to ask for it and show ID. It’s not banned because it’s unsafe. It’s restricted because it’s too effective at boosting blood pressure in people who shouldn’t take it.
If you have uncontrolled hypertension (systolic over 180 or diastolic over 110), pseudoephedrine can trigger a stroke or heart attack. Even if you think you’re fine, check with your doctor before using it.
Phenylephrine may be easier to get, but it’s not safer. It just hides its dangers behind misleading labels and fake effectiveness.
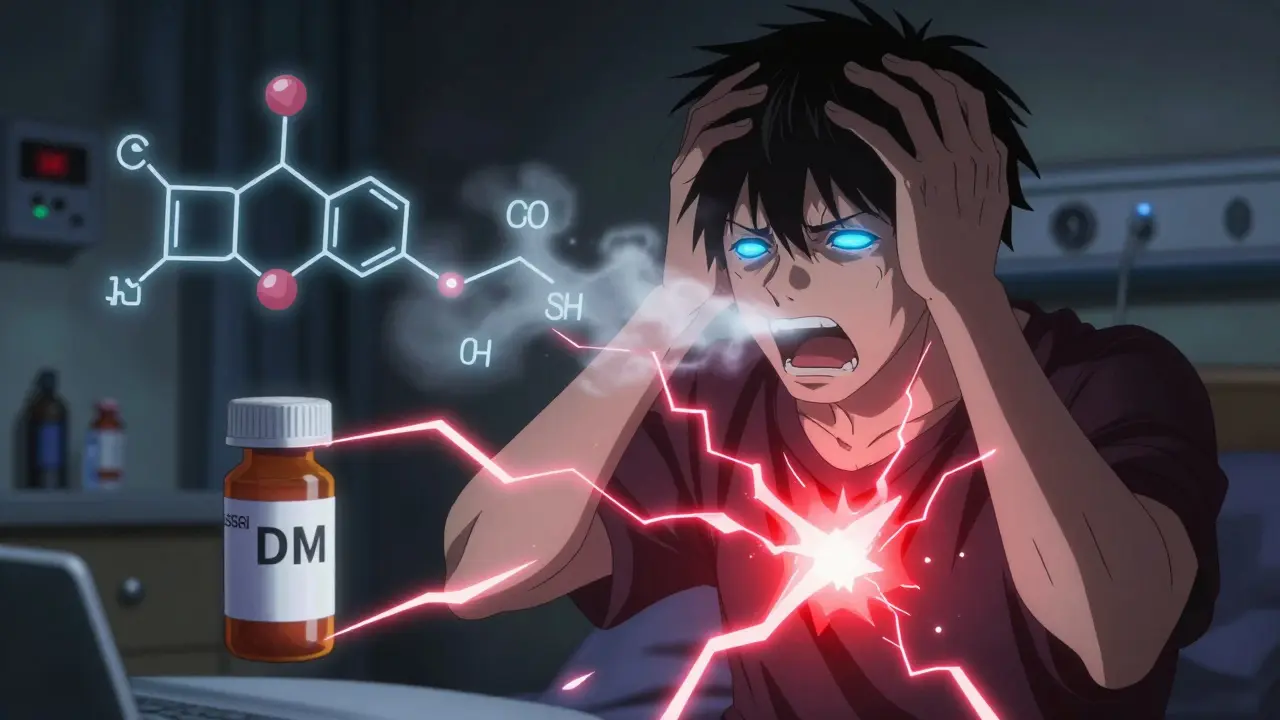
Dextromethorphan and Antidepressants: A Silent Time Bomb
Dextromethorphan (DM) is in almost every cough syrup and cold tablet. It’s not addictive like codeine. But when paired with certain antidepressants? It becomes dangerous.
SSRIs like Prozac, Zoloft, or Lexapro - and SNRIs like Cymbalta or Effexor - are commonly prescribed. If you’re taking one of these and also using a cold medicine with dextromethorphan, you’re increasing your risk of serotonin syndrome.
This isn’t just a theory. A 2017 study in the Journal of Clinical Psychiatry found that combining dextromethorphan with SSRIs raised serotonin syndrome risk by 300%. Symptoms include confusion, rapid heartbeat, high fever, muscle rigidity, and seizures. It can be fatal.
Desert Hope Treatment Center reports that 15% of ER visits involving OTC medication misuse happen because people didn’t realize their cold medicine clashed with their antidepressants. And many of those patients didn’t even tell their doctor they were taking both.
Why You’re Getting It Wrong - And How to Fix It
Here’s what most people do wrong:
- They pick a product because it says “Multi-Symptom Relief” - without checking the ingredients
- They take a cold medicine and a pain reliever, thinking they’re different
- They don’t know what “APAP,” “DM,” or “PE” mean on the label
- They assume “natural” or “non-drowsy” means safer
A 2022 Consumer Reports survey found 41% of people didn’t check all ingredients before buying. That’s not carelessness - it’s confusion.
Here’s how to get it right:
- Read every label - front and back. Look for active ingredients. Ignore the brand names.
- Know the abbreviations: APAP = acetaminophen, DM = dextromethorphan, PE = phenylephrine, PSE = pseudoephedrine.
- Never combine two products with the same active ingredient. If one has acetaminophen, don’t take Tylenol on top of it.
- Ask your pharmacist. They see this every day. Tell them what you’re taking - prescription and OTC.
- Use a drug checker. Apps like Medisafe or WebMD’s Drug Interaction Checker scan barcodes and flag duplicates. WebMD processes over a million checks daily.
And here’s a simple rule: If you only have one symptom - say, just a cough - take a single-ingredient medicine. Don’t force a multi-symptom product on a single problem. You’re adding unnecessary risk.
Who Should Avoid These Medications Altogether?
Some people should never take combination cold and allergy meds without talking to a doctor:
- People with high blood pressure, heart disease, or irregular heartbeat
- People taking MAOIs (like Nardil or Parnate) or tricyclic antidepressants
- People with liver disease - acetaminophen can be toxic
- People with glaucoma, enlarged prostate, or thyroid problems
- Pregnant or breastfeeding women
- Children under 6 - many combination products aren’t approved for them
If you’re unsure, skip the combo. Go for plain antihistamines (like loratadine) for allergies, or plain dextromethorphan for cough. You’ll get relief - without the hidden dangers.
The Bigger Picture: Why This Keeps Happening
The OTC cold and allergy market is worth $8.2 billion in the U.S. alone. Companies make billions selling combination products because they’re easy to market: “One pill for everything!”
But behind the ads, there’s a gap. The FDA hasn’t updated its rules to match modern science. Phenylephrine should’ve been pulled years ago. Acetaminophen limits are too vague on labels. Dextromethorphan interactions aren’t bold enough in warnings.
Meanwhile, 68% of adults use combination products - even when they only have one symptom. That’s not smart. That’s habit.
And it’s costing lives. Emergency room visits linked to OTC medication misuse are rising. The FDA’s own Adverse Event Reporting System shows combination products have 23% more adverse events than single-ingredient ones.
There’s no magic fix. But you can protect yourself. Knowledge is your shield.
Can I take a cold medicine with my blood pressure medication?
It depends on the ingredients. Cold medicines with pseudoephedrine or phenylephrine can raise blood pressure, even if you’re on medication to control it. Always check with your doctor or pharmacist before combining them. If you have high blood pressure, look for products labeled “HBP” (high blood pressure) - these avoid decongestants entirely.
Is it safe to take two different cold medicines at once?
No. Even if they’re different brands, they often contain the same active ingredients. Taking two could mean doubling your dose of acetaminophen or dextromethorphan. That’s how accidental overdoses happen. Always compare ingredient lists - not brand names.
What does APAP mean on a medicine label?
APAP stands for acetaminophen. It’s the chemical abbreviation used on labels to save space. If you see APAP, it’s the same as Tylenol. Many people don’t realize this, which is why they accidentally overdose - taking Tylenol for a headache while already using a cold medicine with APAP.
Can I use OTC cold medicine if I’m on an antidepressant?
Be very careful. Dextromethorphan (DM) in cold medicines can cause serotonin syndrome when taken with SSRIs or SNRIs. Symptoms include confusion, fast heartbeat, fever, and muscle stiffness. If you’re on antidepressants, avoid products with DM. Talk to your doctor before using any OTC cold or allergy medicine.
Are natural or herbal cold remedies safer than OTC meds?
Not necessarily. Many herbal products - like echinacea, zinc, or elderberry - aren’t regulated like drugs. They can still interact with prescription medications or cause side effects. Some herbal remedies contain hidden ingredients that aren’t listed. Stick to FDA-approved OTC medicines with clear labels, and always check for interactions.
