Anaphylaxis from Medication: Emergency Response Steps
 Feb, 17 2026
Feb, 17 2026
When a medication triggers a severe allergic reaction, seconds matter. Anaphylaxis from drugs like penicillin, NSAIDs, or muscle relaxants can turn a routine treatment into a life-or-death emergency. Unlike mild rashes or stomach upset, this is a full-body crisis that shuts down breathing, drops blood pressure, and can kill within minutes. The good news? With the right steps, most cases can be reversed - if you act fast and know exactly what to do.
Recognize the Signs - Don’t Wait for a Rash
Many people think anaphylaxis always starts with hives or swelling. It doesn’t. In fact, 10-20% of medication-induced anaphylaxis cases show no skin symptoms at all. The real warning signs are about your airway, breathing, and circulation - the ABCs.- Difficulty breathing, wheezing, or a persistent cough
- Swelling of the tongue or throat - feels like something’s blocking your airway
- Hoarse voice or trouble talking
- Sudden dizziness, fainting, or collapse
- Pale, clammy skin - especially in children
- Feeling of impending doom
Immediate Action: Lay Them Flat
The first thing you do after recognizing symptoms is not to call 911 - it’s to position the person correctly. This is critical. Allowing someone to stand or walk during anaphylaxis increases the risk of sudden cardiac arrest by 15-20%. The body’s blood pressure plummets, and standing makes it worse - gravity pulls what little blood remains away from the heart and brain.- Have the person lie flat on their back.
- If they’re having trouble breathing, let them sit up with legs stretched out - but don’t let them stand.
- If they’re unconscious or pregnant, roll them onto their left side (recovery position).
- For children, hold them flat - never upright.
Administer Epinephrine - Now
Epinephrine is the only treatment that stops anaphylaxis in its tracks. Antihistamines like Benadryl? They help with itching or hives - but they do nothing for choking, low blood pressure, or shock. Corticosteroids? They’re not needed in most cases and shouldn’t delay epinephrine. Use an auto-injector: EpiPen, Auvi-Q, or Adrenaclick. Inject into the outer thigh - through clothing if needed. Hold it in place for 10 seconds to ensure the full dose goes in. Don’t inject into the arm, buttocks, or hand. Muscle in the thigh absorbs the drug fastest.- Adults and children over 30 kg: 0.3 mg
- Children 15-30 kg: 0.15 mg
Call 911 - Even After Epinephrine
Epinephrine works quickly - within 1-5 minutes - but its effects last only 10-20 minutes. Symptoms can come back harder than before. That’s called a biphasic reaction, and it happens in up to 20% of cases, especially with medication triggers. Calling 911 isn’t optional. It’s mandatory. Emergency responders can give IV fluids, monitor heart rhythm, and deliver more epinephrine if needed. In hospitals, the average time from symptom onset to epinephrine is 8.2 minutes - over the recommended 5-minute window. You can’t afford to wait.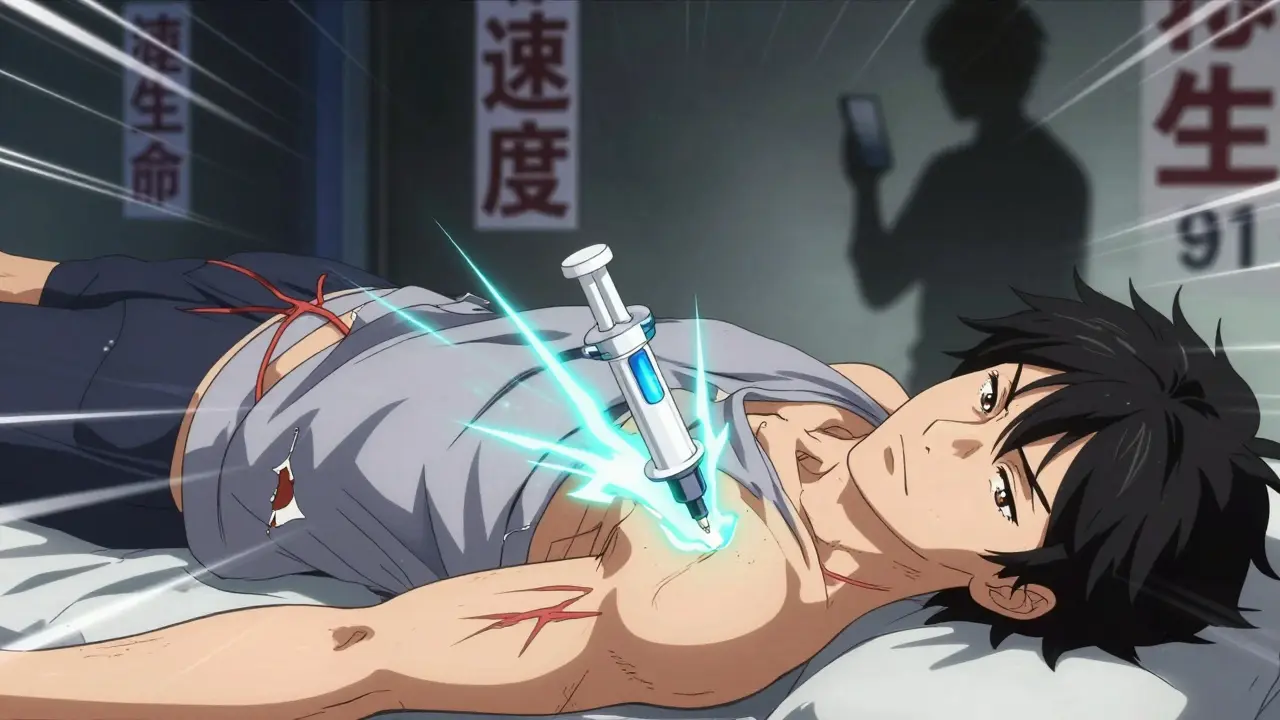
Second Dose? Yes - If Symptoms Return
If breathing or circulation problems don’t improve after 5 minutes, give a second dose of epinephrine. Some guidelines suggest repeating every 5-10 minutes if needed. Don’t wait for a doctor to tell you. If the person is still struggling, give another shot. In severe cases - where two doses don’t help - medical teams may need IV epinephrine. But that’s only done in a hospital, under strict monitoring. You don’t need to know how to do that. Just keep giving IM shots until help arrives.What Not to Do
There are dangerous myths about anaphylaxis. Avoid these at all costs:- Don’t give antihistamines first. They look like a quick fix, but they don’t save lives.
- Don’t wait to see if it gets worse. Anaphylaxis doesn’t wait. Neither should you.
- Don’t let the person stand, walk, or sit upright. Lying flat saves lives.
- Don’t skip the hospital. Even if they seem fine after epinephrine, they need at least 4-6 hours of observation.
Why People Delay - And How to Beat It
In hospitals, 65% of anaphylaxis cases miss the 5-minute epinephrine window. Why? Fear. Nurses and doctors sometimes hesitate because they worry about side effects - rapid heartbeat, high blood pressure. But the risks of not acting are far worse. Out of 35,000 epinephrine doses given for anaphylaxis between 2015-2020, only 0.03% caused serious heart problems. Outside hospitals, many patients carry epinephrine but don’t know how to use it. A 2023 FAACT survey found 29% of people with drug allergies hesitated during a real reaction. Common mistakes:- Not holding the injector in place long enough (37% of users)
- Injecting into fat instead of muscle (18%)
- Using the wrong dose (especially in children)

Special Considerations for Medication-Induced Anaphylaxis
Drug reactions are different from food allergies. People on beta-blockers - common for high blood pressure or heart conditions - may not respond well to standard epinephrine doses. In these cases, higher doses (2-3 times the normal amount) may be needed. If the patient is on beta-blockers, tell emergency responders immediately. Antibiotics cause nearly half of all medication-related anaphylaxis deaths. NSAIDs like ibuprofen or aspirin are next. Even radiocontrast dye used in CT scans can trigger it. If you’ve had a reaction before, carry a medical alert card and avoid the drug forever.After the Emergency
Once stabilized, the patient needs a full allergy workup. This includes:- Referral to an allergist
- Skin or blood testing to confirm the trigger
- Prescription for two epinephrine auto-injectors
- A written emergency action plan
Final Thought: Speed Saves Lives
Anaphylaxis from medication doesn’t care if you’re a doctor, a parent, or a stranger. It doesn’t wait for perfect conditions. It only responds to fast, decisive action. Lay them flat. Give epinephrine. Call 911. Repeat if needed. Don’t second-guess. Don’t delay. You don’t need to be a medical expert - just someone who knows what to do when seconds count.Can antihistamines like Benadryl stop anaphylaxis?
No. Antihistamines may help with mild itching or hives, but they do nothing to reverse airway swelling, low blood pressure, or breathing failure. Giving them instead of epinephrine delays life-saving treatment and increases the risk of death. Always use epinephrine first.
Why is epinephrine injected into the thigh and not the arm?
The thigh muscle (vastus lateralis) has rich blood flow, allowing epinephrine to enter the bloodstream faster than in the arm or buttocks. Studies show IM injection in the thigh reaches peak levels in 8 minutes, compared to 20+ minutes in other sites. Speed is critical in anaphylaxis.
What if I’m not sure if it’s anaphylaxis?
Give epinephrine anyway. The guidelines from the Resuscitation Council UK and ASCIA say: “IF IN DOUBT, GIVE ADRENALINE.” The risks of giving epinephrine are minimal - most side effects like a racing heart are temporary and far safer than letting anaphylaxis progress untreated.
Can you use an expired epinephrine auto-injector?
Yes, if it’s the only option available. While potency declines over time, expired epinephrine still contains active drug. A 2023 study found that even 4 years past expiration, many injectors retained over 80% of their labeled dose. Better to use an expired one than nothing at all.
Why do you need to stay in the hospital for 4-6 hours after anaphylaxis?
About 20% of anaphylaxis cases have a biphasic reaction - meaning symptoms return hours later, sometimes worse than before. This is more common with medication triggers than food. Observation allows medical teams to catch and treat a second wave before it becomes life-threatening.

Irish Council
February 17, 2026 AT 18:22Done.