Antidepressants and Alcohol: What You Need to Know About the Dangerous Mix
 Feb, 14 2026
Feb, 14 2026
Antidepressant-Alcohol Safety Checker
This tool provides general guidance about alcohol and antidepressant interactions based on medical research and guidelines. It is NOT a substitute for professional medical advice. Always consult your doctor before making decisions about alcohol consumption while taking antidepressants.
When you're taking antidepressants, your brain is already working hard to rebalance chemicals that control mood, sleep, and energy. Adding alcohol into the mix doesn't just dull the effects-it can turn a treatment into a threat. This isn't a "maybe" or "sometimes." It's a clear, documented risk that can lead to hospitalization, worsened depression, or even death. If you're on antidepressants and wondering if one drink is okay, the answer isn't what you might hope for.
Why Alcohol and Antidepressants Don't Mix
Alcohol is a depressant. That means it slows down your central nervous system. Antidepressants, on the other hand, are designed to lift your brain out of depression by adjusting neurotransmitters like serotonin, norepinephrine, and dopamine. When you mix them, it's like trying to drive a car while someone keeps hitting the brakes and the gas at the same time. The result? Chaos. The problem isn't just one-size-fits-all. Different types of antidepressants react differently with alcohol, but every single class has dangerous outcomes. A 2022 meta-review found that nearly 80% of deaths linked to antidepressant use involved alcohol. Most of those were suicides. That’s not a coincidence. Alcohol lowers your inhibitions, increases impulsivity, and makes depressive thoughts feel louder and more urgent.How Different Antidepressants React with Alcohol
SSRIs like Prozac, Zoloft, and Lexapro are the most commonly prescribed. They’re safer than older drugs-but not safe with alcohol. When you drink while on an SSRI, your body processes alcohol differently. You get drunk 30-50% faster. One beer might feel like three. That’s not just about feeling dizzy. It’s about losing control. A Reddit user on r/mentalhealth described how one beer left them vomiting and dizzy for 12 hours. That’s not normal intoxication-that’s a reaction. Tricyclic antidepressants like amitriptyline are older but still used. They make alcohol’s sedative effects way worse. People on these drugs have been found to have respiratory depression at blood alcohol levels as low as 0.05%-that’s less than one drink for most people. Falls, accidents, and unconsciousness become far more likely. Studies show users on TCAs are over three times more likely to fall or get injured when drinking compared to drinking alone. MAOIs like Nardil and Parnate are rare today, but they’re the most dangerous. These drugs block an enzyme that breaks down tyramine, a chemical found in beer, wine, and aged cheese. When alcohol hits your system, it can cause a sudden, massive spike in blood pressure-sometimes over 220/120 mmHg. That’s a hypertensive crisis. It can trigger a stroke or heart attack within 30 minutes. This isn’t a myth. It’s documented in emergency rooms across the U.S. Wellbutrin (bupropion) is different. It doesn’t affect serotonin. Instead, it boosts dopamine and norepinephrine. When alcohol is added, it can flood your brain with dopamine. That sounds good-until it doesn’t. People have reported hearing voices, believing they’re being watched, or having violent urges. FHE Health’s 2022 data shows 12% of patients who mixed Wellbutrin and alcohol ended up in the ER with psychosis-like symptoms. One patient on PatientsLikeMe wrote: "Two glasses of wine, and I started hearing voices telling me to hurt myself. I was hospitalized for 24 hours."The Hidden Cost: Reduced Effectiveness
Even if you don’t feel "drunk" or "sick," alcohol is still sabotaging your treatment. Research from Alcohol Help found that just one standard drink per day cuts antidepressant effectiveness by 35-50% in 78% of users. That means your medication isn’t working as well. You might think you’re fine-but your depression is creeping back. A 2021 study in the Journal of Clinical Psychiatry showed people who avoided alcohol while on antidepressants had a 62% higher chance of full remission. That’s huge. But here’s the kicker: NAMI’s 2022 survey found most patients never hear this. Doctors focus on side effects, not outcomes. You’re told not to drink because it’s "unsafe," but not that quitting alcohol could be the single biggest step toward feeling better.
What Experts Really Say
Dr. David Baron from FHE Health says mixing Wellbutrin and alcohol can cause symptoms "resembling psychosis"-a condition that requires hospitalization. Dr. Mark Gold from American Addiction Centers warns alcohol can "potentiate suicide risk," citing a 2.7 times higher risk in patients who drink while on antidepressants. But there’s nuance. Dr. Michael Thase, a top psychiatrist, notes in his 2023 textbook that for stable patients on SSRIs after 8-12 weeks of successful treatment, "occasional, moderate alcohol consumption may be acceptable"-but only with doctor approval and careful monitoring. The American Psychiatric Association’s 2023 guidelines now allow for one drink per week for some patients on SSRIs, but only if they have no history of alcohol abuse and are under regular care. Still, the majority of medical organizations-including the National Institute on Alcohol Abuse and Alcoholism (NIAAA)-recommend complete abstinence. Why? Because the margin for error is too small. One drink might be fine for one person, but deadly for another. And you won’t know which one you are until it’s too late.Real People, Real Consequences
Look at the data from real users. The Depression and Bipolar Support Alliance surveyed 4,312 people. 67% said their depression got worse within 48 hours of drinking. 29% said their anxiety spiked. 42% said they couldn’t work because of extreme drowsiness. 28% reported intensified suicidal thoughts. One Drugs.com review from May 2023 said: "My doctor allows one glass of wine weekly with my Lexapro and I’ve had no issues in 18 months." That’s the exception. Out of 12,000 medication reviews analyzed by Addiction Center, only 3% reported no negative effects. The rest? Dizziness, nausea, emotional outbursts, or worse.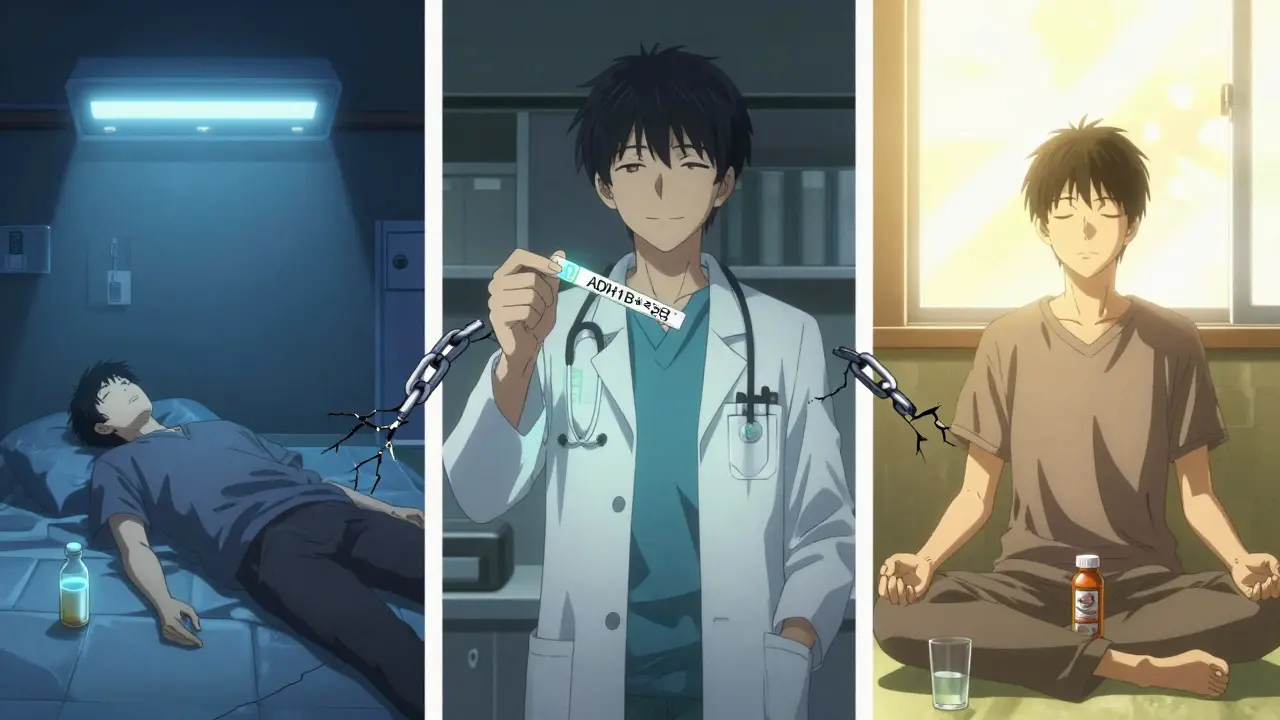
What Should You Do?
If you’re just starting antidepressants, don’t drink at all. The first 4-8 weeks are critical. Your body is adjusting. Alcohol interferes with that process. It can make side effects worse and delay improvement. If you’ve been stable for months or years, talk to your doctor. Don’t assume it’s okay. Ask: "Is my specific medication safe with alcohol? Do I have any risk factors?" Some people can handle one drink once a week. Others can’t handle even a sip. If you use alcohol to cope with anxiety or sadness, that’s a red flag. A 2022 Columbia Recovery Center survey found 39% of antidepressant users drink to self-medicate. That’s not treatment-it’s a cycle. Cognitive behavioral therapy for alcohol use has a 47% success rate in helping these patients cut back, according to a 2021 JAMA Psychiatry study.What’s Changing Now?
In March 2023, the FDA approved the first genetic test-GeneSight Psychotropic-that can tell you how your body metabolizes alcohol and antidepressants. Some people have a gene variant (ADH1B*2) that makes them 2.3 times more sensitive to the combo. That’s not theoretical. It’s measurable. Hospitals and clinics are now required to educate patients on this interaction. 78% of treatment centers include it in their onboarding. But here’s the problem: only 41% of patients actually receive the materials. Warning labels are on every bottle now, but if you don’t read them-or your doctor doesn’t explain them-you’re still at risk.Bottom Line
This isn’t about being perfect. It’s about being smart. If you’re on antidepressants, alcohol isn’t just a social drink. It’s a medical risk. Even one drink can make you sicker, more suicidal, or less responsive to treatment. The safest choice? Avoid it entirely. If you’re considering drinking, talk to your doctor first. And if you’re using alcohol to numb your pain, seek help-not just for your depression, but for the drinking too. Your brain is fighting hard to heal. Don’t let alcohol undo it.Can I have one drink while on antidepressants?
For most people, the answer is no. Even one standard drink-like a 12-ounce beer or 5-ounce glass of wine-can worsen side effects, reduce medication effectiveness, and increase suicide risk. A few stable patients on SSRIs after 12+ weeks of treatment may be allowed one drink per week with doctor approval, but this is rare and requires careful monitoring. For everyone else, abstinence is the safest path.
Does alcohol make antidepressants less effective?
Yes. Research shows that even one drink per day reduces antidepressant effectiveness by 35-50% in 78% of users. Alcohol interferes with how your brain responds to the medication, which can delay recovery or cause symptoms to return. It also lowers adherence-people who drink are more likely to skip doses or stop treatment entirely.
What happens if I drink while on Wellbutrin?
Drinking while on Wellbutrin (bupropion) can trigger dopamine flooding in the brain, leading to psychosis-like symptoms such as auditory hallucinations, delusions, and intense paranoia. In 12% of documented cases, this requires emergency hospitalization. FHE Health reports that one in eight patients who combine Wellbutrin with alcohol experience these severe reactions. It’s not just "feeling weird"-it’s a medical emergency.
Is it safe to drink alcohol if I’ve been on antidepressants for years?
Not necessarily. Long-term use doesn’t eliminate the risk. Your body’s response to alcohol doesn’t change just because you’ve been on medication for years. Some people may tolerate minimal alcohol, but others can still experience dangerous interactions. Always consult your doctor before drinking-even if you feel fine. Your brain chemistry is still vulnerable to alcohol’s effects.
Can I switch to a different antidepressant to avoid this problem?
All antidepressants interact with alcohol in some way. While SSRIs are generally considered lower risk than MAOIs or Wellbutrin, no class is completely safe. Switching medications won’t solve the issue unless you also stop drinking. The real solution isn’t changing pills-it’s removing alcohol from the equation. If you’re struggling to quit drinking, talk to your doctor about integrated treatment options.
