Autoimmune Disease Monitoring: Lab Markers, Imaging, and Visits
 Dec, 7 2025
Dec, 7 2025
When you live with an autoimmune disease, feeling okay one week and crashing the next isn’t just bad luck-it’s a sign your body’s immune system is switching gears. The goal isn’t just to treat symptoms when they show up. It’s to catch those switches early, before your joints swell, your kidneys struggle, or your skin breaks out in angry rashes. That’s where autoimmune disease monitoring comes in. It’s not optional. It’s the difference between managing your condition and letting it manage you.
Lab Markers: What Your Blood Is Telling You
Your blood isn’t just red fluid. It’s a live report card on your immune system. Three key markers are tracked at nearly every visit: CRP, ESR, and autoantibodies.
C-reactive protein (CRP) rises fast when inflammation flares. Levels above 3.0 mg/L are a red flag. It’s not perfect-exercise, infection, or even stress can nudge it up-but when it spikes from your baseline, something’s burning inside. Erythrocyte sedimentation rate (ESR) measures how quickly red blood cells sink in a tube. Over 20 mm/hr for women, 15 mm/hr for men? That’s slow sinking, and it usually means chronic inflammation. Both tests are cheap, fast, and widely available.
But the real stars are the autoantibodies. The ANA test is the first screen. If it’s positive, it doesn’t mean you have lupus-it means your immune system is making antibodies against your own cells. About 20% of healthy people test positive. That’s why ANA alone isn’t a diagnosis. But when it’s positive and you have symptoms, it’s the starting gun.
That’s when reflex testing kicks in. If ANA is positive, labs check for specific antibodies like anti-dsDNA, which shows up in 60-70% of lupus cases and rises when kidney involvement (lupus nephritis) flares. Anti-SSA and anti-SSB point to Sjögren’s syndrome. Scl-70 is a marker for systemic sclerosis. Jo-1? That’s polymyositis. These aren’t just labels-they’re clues to what’s happening in your body right now.
Don’t get fooled by repeated ANA tests. Once positive, it usually stays positive-even in remission. That’s why doctors watch complement levels (C3 and C4) instead. When they drop, it means your immune system is consuming them to attack your tissues. That’s active disease.
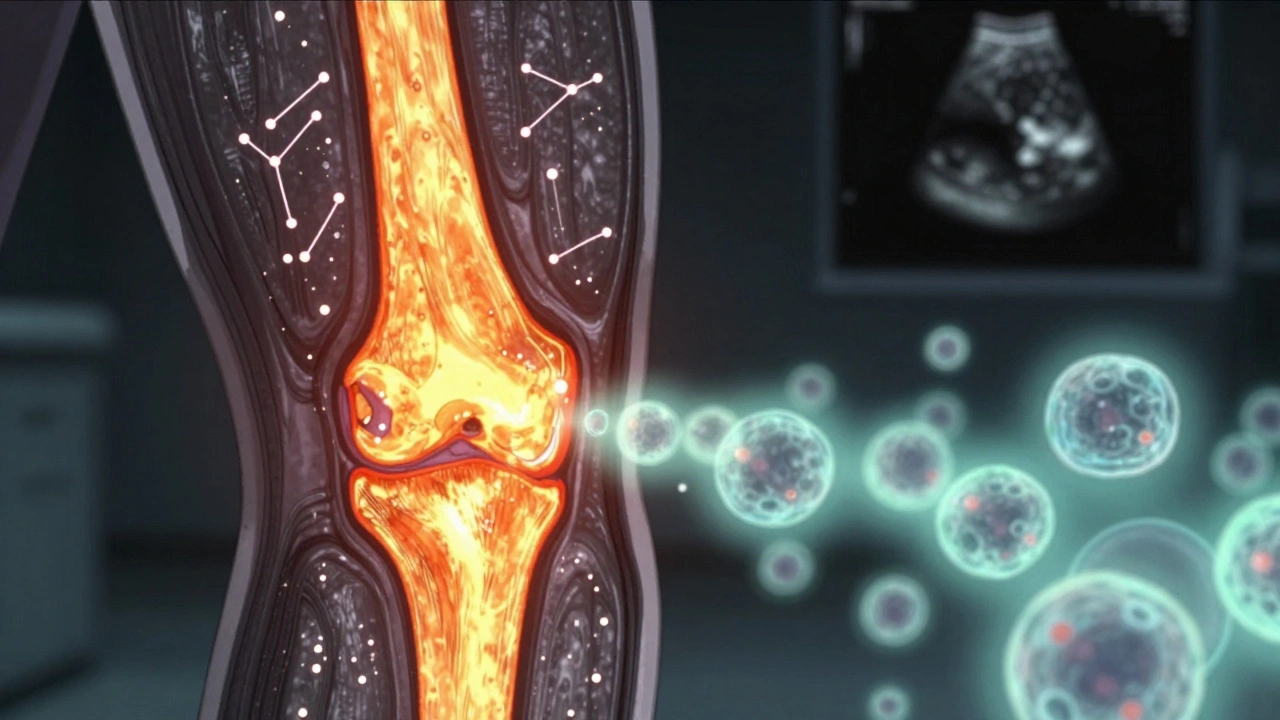
Imaging: Seeing What Blood Can’t Show
Lab tests tell you something’s wrong. Imaging tells you where and how bad. And sometimes, it shows damage before you even feel it.
MRI is the gold standard for soft tissue. It can spot inflammation in joints, tendons, and even the brain long before X-rays show erosion. Newer contrast agents are safer and more targeted, avoiding the risks of old gadolinium-based dyes. For rheumatoid arthritis, ultrasound with microbubble contrast can measure blood flow in inflamed joints with 85% accuracy. It’s real-time, non-invasive, and doesn’t use radiation.
PET scans are changing the game. By tagging immune cells with radioactive tracers, doctors can see where T-cells are gathering-like a heat map of your body’s internal war. This isn’t routine yet, but in research centers, it’s helping predict flares and measure how well new drugs quiet the immune system.
SPECT scans use radiolabeled peptides to light up specific inflammation sites. They’re not as sharp as MRI, but they show molecular activity, not just structure. CT scans are used when there’s concern about lung or organ damage, especially in scleroderma or vasculitis.
Here’s the catch: not all imaging is created equal. A joint MRI done in a general radiology clinic might miss early changes that a rheumatology-specialized center catches. Location matters. So does timing. Imaging every 6 months isn’t always needed-unless you’re in a flare or starting a new drug.
Clinical Visits: The Human Piece of the Puzzle
No machine can replace a doctor who listens. That’s why structured visits are non-negotiable.
When you’re first diagnosed, expect visits every 4 to 6 weeks. That’s when meds are being adjusted, side effects are being watched, and labs are being checked. Once things stabilize, you’ll usually shift to every 3 to 4 months. The American College of Rheumatology says you need at least two full assessments a year-labs, physical exam, and your own report on how you’re feeling.
Doctors use scoring systems to track progress. For rheumatoid arthritis, it’s DAS28. For lupus, it’s SLEDAI. These aren’t just numbers-they combine joint counts, fatigue levels, lab values, and patient input into one score. If your DAS28 drops from 5.8 to 2.3, that’s not luck. That’s treatment working.
But here’s what most people miss: 63% of flares show up first in how you feel-not in your blood. You might say, “My hands are stiff in the morning,” or “I can’t climb stairs like I used to.” That’s data. That’s just as important as a CRP level. Relying only on labs is like driving with blinders on.
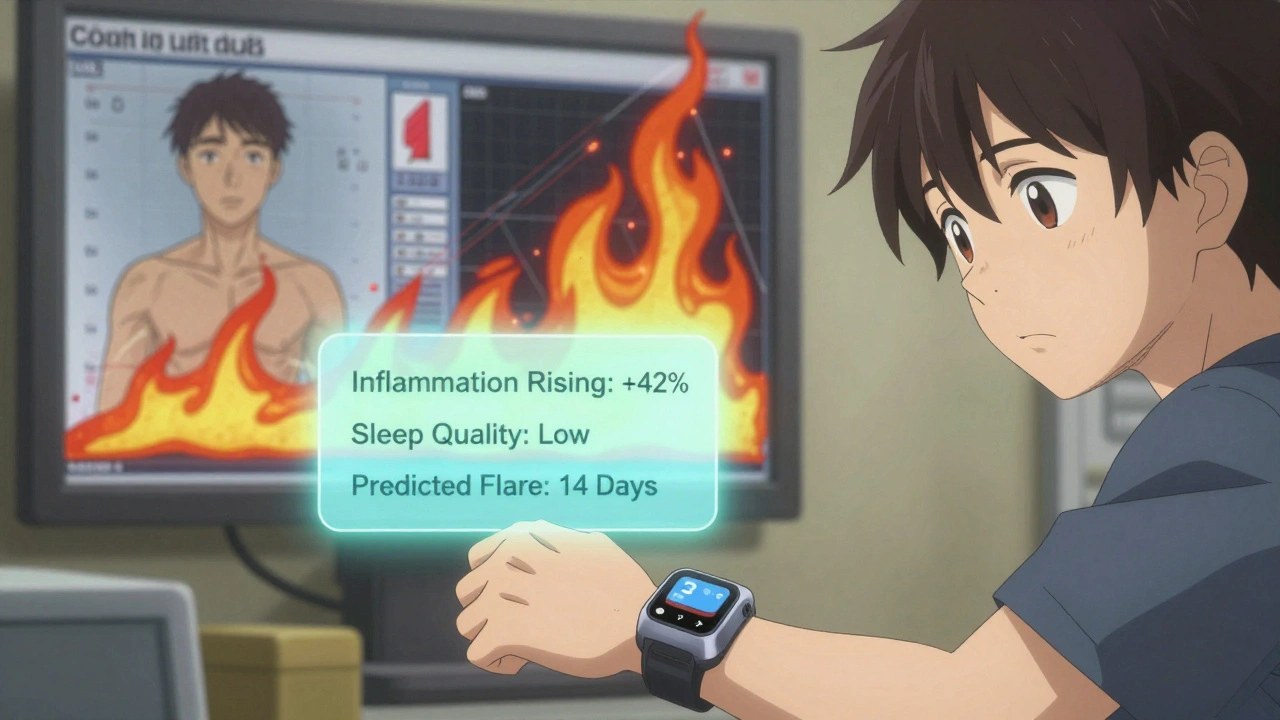
What’s New: Wearables, AI, and Digital Tracking
The future isn’t just in the lab or the scanner. It’s in your pocket.
Wearables are now testing interstitial fluid for inflammatory markers. Early studies show they match traditional CRP readings 89% of the time. Imagine getting a notification: “Your inflammation is rising. Schedule a check-up.” That’s not sci-fi-it’s happening now.
AI tools are learning your pattern. By analyzing your past lab results, symptom logs, and even sleep data, some platforms predict flares 14 days in advance with 76% accuracy. The FDA approved the first such system, AutoimmuneTrack, in mid-2023. In a trial of over 2,300 patients, emergency visits dropped by 29% in just one year.
These tools don’t replace doctors. They give them better data. And they give you more control. If you’re logging your fatigue, pain, and sleep every day, your doctor can see trends you never noticed.
Barriers and Real-World Challenges
Not everyone gets the care they need.
Test results vary wildly between labs. ANA results can differ by 22% just because of how the test was run. Insurance won’t always cover monthly MRIs or advanced antibody panels. Medicaid patients are less than half as likely to get recommended monitoring as those with private insurance.
Cost isn’t the only hurdle. Time is too. Taking off work for a 3-hour appointment every 3 months isn’t easy if you’re hourly or caring for kids. That’s why some clinics now offer hybrid visits-some labs done locally, some check-ins by video, with imaging scheduled only when needed.
And yet, patients who stick with structured monitoring report 68% better outcomes. They’re less likely to end up in the hospital. Less likely to need stronger drugs. Less likely to lose function.
What You Should Do Right Now
Don’t wait for a flare to act.
- Ask your doctor: “What are my key lab markers, and what numbers should I watch?”
- Keep a simple symptom log: pain level (1-10), fatigue, stiffness, new rashes. Use a phone app or even a notebook.
- Know your baseline. If your CRP was 1.2 last year and now it’s 4.8, that’s a signal.
- Ask about imaging. “Could an ultrasound or MRI help us see what’s going on under the surface?”
- Push back if you’re told “your ANA is positive, so that’s it.” ANA doesn’t track activity. Complement levels do.
- Check if your clinic uses a disease activity score. If not, ask why.
Autoimmune diseases don’t follow calendars. But your monitoring schedule should. The goal isn’t perfection. It’s awareness. It’s catching the fire before it becomes a wildfire.
Do I need to get ANA tests repeatedly to monitor my autoimmune disease?
No. Once ANA is positive, it usually stays positive-even when your disease is in remission. Repeating it doesn’t tell you if you’re flaring or improving. Instead, doctors track complement levels (C3 and C4), CRP, ESR, and disease-specific antibodies like anti-dsDNA for lupus. These change with activity and give real-time insight.
How often should I have imaging done for my autoimmune condition?
It depends on your disease and how stable you are. If you’re newly diagnosed or in a flare, imaging like MRI or ultrasound may be done every 3-6 months to track inflammation. Once stable, you might only need imaging once a year-or even less-if you’re not having new symptoms. Always ask: “What are we looking for, and how will this change my treatment?”
Can wearable devices replace lab tests for autoimmune monitoring?
Not yet. Wearables that track inflammation through skin fluid are promising and correlate well with CRP levels, but they’re still experimental. They’re best used as early warning tools, not replacements. Lab tests still provide the definitive numbers doctors need to make treatment decisions. Think of wearables as your personal alarm system-not your diagnostic tool.
Why do some doctors skip imaging and only rely on blood tests?
Cost, access, and habit. Imaging is expensive, not always covered by insurance, and requires scheduling. Many clinics still rely on labs because they’re fast and cheap. But this approach misses up to 40% of early tissue damage. If your symptoms don’t match your lab results, push for imaging. You’re not being difficult-you’re being smart.
Is there a difference between monitoring for lupus vs. rheumatoid arthritis?
Yes. Lupus monitoring focuses on anti-dsDNA, complement levels (C3/C4), and urine tests for kidney involvement. Rheumatoid arthritis uses DAS28 scores, joint ultrasound, and CRP/ESR. While both use similar inflammation markers, the specific antibodies and imaging targets differ. Your monitoring plan should be tailored to your diagnosis-not copied from someone else’s.
What should I bring to my autoimmune monitoring appointment?
Your symptom log (even a simple list), a list of all medications and supplements, any recent lab results you’ve received, and a note on how your daily life has changed-sleep, energy, pain, mobility. The more detail you give, the better your doctor can adjust your plan. Don’t wait until you’re having a bad day to speak up.

Ruth Witte
December 8, 2025 AT 00:16OMG YES THIS! 🙌 I started tracking my fatigue and pain in a little app and wow-my flare happened 10 days before my CRP spiked. My rheum doc was SHOCKED. Wearables + logs = game changer. Don’t wait until you’re bedridden to speak up! 💪
Noah Raines
December 9, 2025 AT 21:32Been there. Got the t-shirt. ANA positive since 2018 and still here. No one ever told me to watch C3/C4 until I read this. Thanks for spelling it out. I’ve been asking for those since last year. Now I just need insurance to pay for the damn tests 😅
Gilbert Lacasandile
December 11, 2025 AT 06:06This is actually really helpful. I’ve been skipping my 3-month visits because I feel fine, but now I get why that’s dangerous. I’m scheduling mine for next week. Maybe I’ll start a symptom log too. Small steps, right?
Lola Bchoudi
December 12, 2025 AT 01:28As a rheumatology nurse practitioner, I can’t stress this enough: DAS28 and SLEDAI aren’t just bureaucratic checkboxes-they’re quantitative measures of disease burden. When patients come in with a symptom log and baseline labs, we can titrate biologics with precision. Don’t underestimate the power of granular data. Your body’s whispering-listen before it screams.
Morgan Tait
December 13, 2025 AT 13:08They’re hiding the truth. Labs? Imaging? Wearables? All controlled by Big Pharma to keep you dependent. The real solution is vitamin D, magnesium, and avoiding 5G towers. I’ve been symptom-free for 7 years since I stopped trusting doctors. They inject you with toxins to make you need more meds. Look up the Pizzagate connection to rheumatoid arthritis-it’s all linked.
Christian Landry
December 14, 2025 AT 08:56wait so u mean i dont need to get my ana tested every time? i thought that was the main thing?? 😅 thanks for clearing that up. i’ve been asking for it like a broken record. gonna start asking for c3/c4 now. also, i’ve been using a notes app for pain levels and it’s kinda helping. not perfect but better than nothing lol
Katie Harrison
December 16, 2025 AT 06:16I appreciate this post. Truly. But I also want to acknowledge that for many of us-especially in rural areas or without reliable transportation-getting a monthly MRI or even a lab draw is a logistical nightmare. Hybrid visits are a step forward, but we need more than ‘suggestions.’ We need policy change. Thank you for the info. I’ll use it. But please don’t pretend access is equal.
Michael Robinson
December 16, 2025 AT 11:26It’s not about the numbers. It’s about knowing your body. The machine can’t feel your stiffness at 6 a.m. or the way your breath catches when you stand up. Monitoring isn’t science-it’s listening. And listening takes time. And time is the one thing we’re never given.
Kathy Haverly
December 17, 2025 AT 19:33Wow. So you’re telling me I should trust a system that misdiagnosed me three times, lost my lab results twice, and told me my pain was ‘all in my head’? You want me to log my suffering so they can charge me $400 for a ‘follow-up’? No thanks. I’ll just keep medicating myself and avoiding the system. You’re selling a lie wrapped in graphs.
Noah Raines
December 17, 2025 AT 21:06@5703 I get it. I’ve been there too. But I tried the ‘ignore it’ route. Ended up in the ER with pericarditis. This stuff doesn’t wait. I still hate the system. But now I use it like a weapon-get the data, push back, demand better. It’s not perfect. But it’s better than dying quietly.