Clozapine and Smoking: How CYP1A2 Induction Affects Dose Needs
 Dec, 27 2025
Dec, 27 2025
Clozapine Dose Adjustment Calculator
This tool helps clinicians adjust clozapine doses based on smoking status changes. Always follow therapeutic drug monitoring guidelines.
Important: This calculator provides general guidance only. Always verify with therapeutic drug monitoring (TDM) and follow clinical guidelines.
When someone takes clozapine for treatment-resistant schizophrenia, their smoking habit isn’t just a personal choice-it’s a medical factor that can make the difference between effective treatment and dangerous side effects. This isn’t theoretical. It’s happening in clinics every day. Smokers often need clozapine doses that are 50% to 100% higher than non-smokers just to stay stable. And if they quit smoking? Their blood levels can spike overnight, leading to confusion, rapid heartbeat, seizures, or worse.
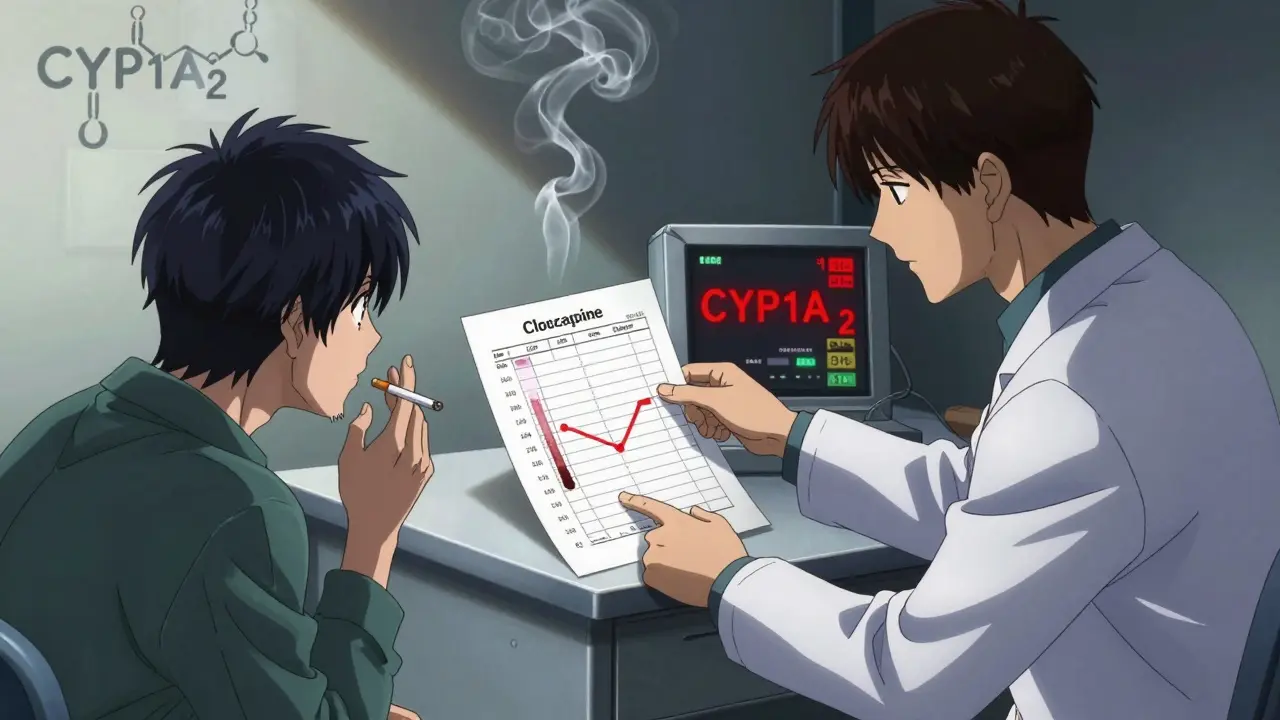
Why Smoking Changes How Clozapine Works
Clozapine is broken down in the liver by one enzyme: CYP1A2. That’s it. Unlike other antipsychotics that use multiple pathways, clozapine relies almost entirely on this one. And cigarette smoke? It’s a powerful trigger for CYP1A2. The chemicals in smoke-especially polycyclic aromatic hydrocarbons (PAHs)-tell your liver to make more of this enzyme. More enzyme means faster breakdown of clozapine. That’s why smokers clear the drug so quickly.Studies show that smokers on clozapine have serum concentrations that are about 2.5 times lower than non-smokers taking the same dose. One 2003 study found smokers needed an average of 382 mg per day, while non-smokers did fine on 197 mg. That’s not a small difference. That’s a doubling. And if you don’t adjust for it, the patient isn’t getting enough medication. Their psychosis returns. Their hospitalization risk goes up.
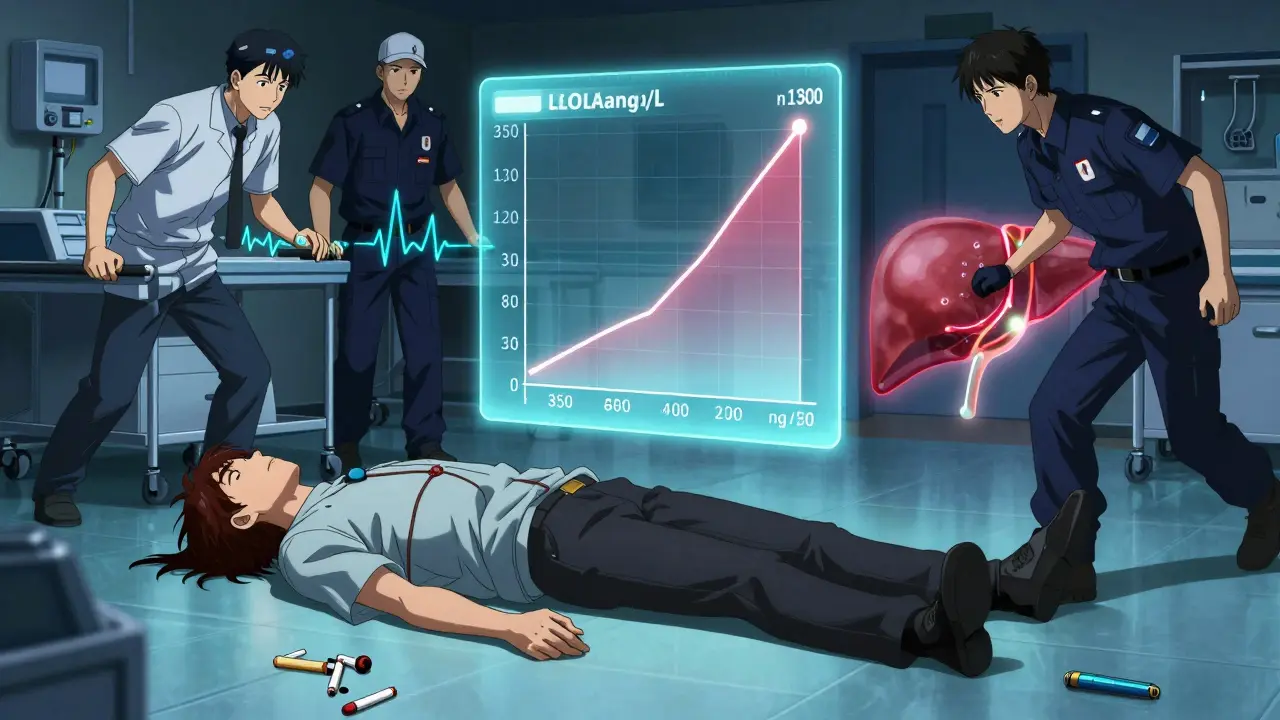
What Happens When Someone Stops Smoking
Quitting smoking doesn’t just improve lung health-it can be a medical emergency for someone on clozapine. The CYP1A2 enzyme doesn’t shut off instantly. It takes time to wind down. But within 48 hours, activity starts dropping. By day 7, it’s down by about 36%. That means clozapine starts building up in the blood.Research shows that, on average, clozapine levels rise by 29.3% within two weeks after quitting. But averages don’t tell the whole story. Some people see a 10% increase. Others? Their levels jump over 200%. One case report described a 45-year-old man whose clozapine level soared to 1,200 ng/mL-more than double the safe upper limit-just 10 days after he stopped smoking. He ended up in intensive care.
That’s why guidelines now say: as soon as someone quits smoking, reduce their clozapine dose by 25% to 30%. Don’t wait. Don’t assume they’ll be fine. Monitor their blood levels weekly for at least two weeks. If you don’t, you’re playing Russian roulette with their safety.
Vaping Isn’t a Safe Alternative
A lot of people switch from cigarettes to vaping thinking it’s harmless. It’s not. While vaping doesn’t contain the same PAHs that strongly induce CYP1A2, it’s not neutral either. Some vape liquids have aldehydes and carbonyls that can still affect liver enzymes. The result? Unpredictable clozapine levels.One study found that switching from smoking to vaping led to higher clozapine concentrations-sometimes enough to cause toxicity. But in other cases, levels dropped, possibly due to other compounds in vape juice. There’s no consistent pattern. That means if a patient switches to vaping, you can’t assume their dose is still right. You need to check their blood levels just like you would after quitting smoking.
Genetics Don’t Save You
You might think some people are naturally more sensitive to this interaction because of their genes. After all, CYP1A2 has a known variant-CYP1A2*1F-that affects how the enzyme responds to inducers. But here’s the twist: the 2003 study that first highlighted the smoking-clozapine gap tested 80 patients and found no link between this gene variant and dose needs. Smokers with the “high-inducibility” gene didn’t need higher doses than smokers without it. Non-smokers with the gene didn’t need lower doses.What matters most isn’t your DNA. It’s your behavior. Whether you smoke 1 cigarette or 20 a day, whether you quit yesterday or 10 years ago-that’s what changes your clozapine levels. That’s why clinical guidelines focus on smoking status, not genetic testing. The only reliable tool? Therapeutic drug monitoring (TDM).
Therapeutic Drug Monitoring Isn’t Optional
Clozapine has a narrow therapeutic window: 350 to 500 ng/mL. Below that? Risk of relapse. Above that? Risk of seizures, heart inflammation, or agranulocytosis. You can’t guess the right dose. You can’t rely on weight, age, or how they “look.” You need to measure the drug in their blood.For smokers, the concentration-to-dose ratio (C/D) is usually below 0.8 (ng/mL per mg/day). For non-smokers, it’s 1.5 to 2.0. That’s a huge gap. If your patient is smoking and their C/D is 1.2, they’re probably underdosed. If they quit smoking and their C/D jumps to 2.5? They’re overdosed.
Guidelines from the American Psychiatric Association and the Dutch Pharmacogenetics Working Group say TDM is mandatory for all clozapine users. And it’s not a one-time test. You need it before any dose change, and again 10 days after-because that’s how long it takes for levels to stabilize. If you’re not doing TDM, you’re not managing clozapine safely.
What About Coffee?
Caffeine is also metabolized by CYP1A2. Heavy coffee drinkers-three or more cups a day-can have slightly higher enzyme activity. That means they might need 15% to 20% more clozapine than non-coffee drinkers, even if they don’t smoke. It’s a smaller effect than smoking, but it adds up. If someone quits smoking and also cuts back on coffee? Their clozapine levels could rise even faster. You have to ask about both.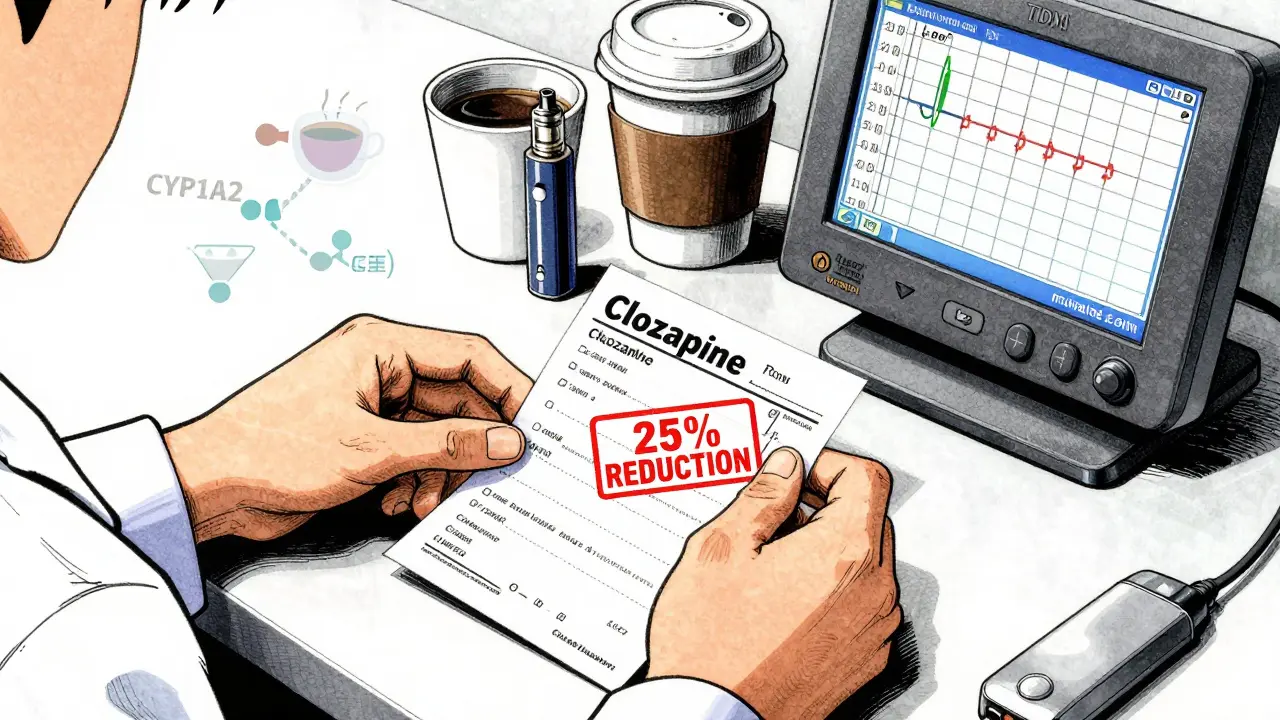
Real Consequences, Real Stories
On Reddit’s psychiatry forum, clinicians shared stories: three patients in 2022 developed delirium and tachycardia within days of quitting smoking. Their clozapine levels went from 350 ng/mL to over 800 ng/mL. One patient had to be sedated. Another nearly had a seizure.But there are good stories too. One patient in a 2021 study quit smoking and worked with their doctor to reduce their clozapine dose from 450 mg to 250 mg over 10 days, using weekly blood tests. No side effects. No relapse. Just careful management.
The difference? One team was watching the numbers. The other wasn’t.
What You Need to Do
Here’s the practical checklist for anyone managing clozapine:- Ask about smoking status at every visit. Don’t assume. Ask again if they’ve been hospitalized or changed living situations.
- If they smoke, start clozapine at the standard dose but expect to increase it by 50-100% within a few weeks. Use TDM to guide this.
- If they quit smoking, reduce the dose by 25-30% immediately. Monitor levels weekly for 2-3 weeks.
- If they switch to vaping, treat it like a smoking cessation. Check levels after two weeks.
- Ask about caffeine intake. High coffee drinkers may need slightly higher doses.
- Never adjust dose without TDM. Not even if they “feel fine.”
And if you’re not doing TDM? Start now. The cost of a single avoidable hospitalization due to clozapine toxicity is over $12,500. The human cost? Much higher.
What’s Next?
Researchers are working on faster, cheaper ways to measure CYP1A2 activity. One trial is testing caffeine metabolism as a point-of-care biomarker-like a breathalyzer for liver enzyme activity. It’s still in testing, but it could one day replace blood draws with a simple urine or saliva test.Meanwhile, drug companies are exploring new clozapine formulations that don’t rely on CYP1A2. That could be a game-changer. But until then, the rule is simple: know their smoking status. Measure their blood levels. Adjust their dose. Don’t guess. Don’t delay. Lives depend on it.

Elizabeth Ganak
December 28, 2025 AT 18:22Wow, this is such a crucial post. I work in psych outreach and we’ve had two patients crash after quitting smoking without warning. TDM isn’t optional-it’s life or death. Thanks for laying it out so clearly.
Nicola George
December 29, 2025 AT 11:40So let me get this straight… you’re telling me my cousin’s ‘vape habit’ is basically a silent drug interaction waiting to blow up? 🤦♀️
Nikki Thames
December 29, 2025 AT 13:08While I appreciate the clinical precision of this exposition, one must consider the ethical implications of reducing patients’ autonomy under the guise of pharmacological necessity. Are we, as clinicians, pathologizing behavioral choices that, while medically consequential, remain deeply personal? The reduction of smoking cessation to a mere pharmacokinetic variable risks dehumanizing those we seek to heal.
Olivia Goolsby
December 30, 2025 AT 09:03Let’s be real-this whole CYP1A2 thing is just a distraction. Big Pharma doesn’t want you to know that clozapine’s real danger comes from the government’s secret fluoride program in the water supply, which synergistically amplifies liver enzyme suppression. That’s why the ‘dose adjustments’ are so inconsistent. They’ve been hiding this since 1998! The FDA knows. The AMA knows. And yet… silence. Check your blood. Check your tap. Check your soul.
Elizabeth Alvarez
December 30, 2025 AT 11:52And nobody’s talking about the fact that the entire psychiatric establishment is built on this lie? CYP1A2? Please. The real reason smokers need higher doses is because the pharmaceutical industry designed clozapine to be dependent on nicotine to keep patients hooked-literally. They profit from both the addiction and the dose escalation. It’s not science-it’s a business model. And now they’re pushing ‘vaping is unsafe’ to sell more blood tests? Wake up.
Liz MENDOZA
December 31, 2025 AT 05:51I’m a nurse on the inpatient psych unit, and I’ve seen this play out too many times. One patient went from 400mg to 150mg after quitting cold turkey-no warning, no monitoring. He had a seizure in the shower. We barely got him stabilized. This isn’t theory. It’s our daily reality. Thank you for saying this out loud.
Monika Naumann
January 2, 2026 AT 01:36It is unfortunate that Western medicine continues to prioritize biochemical reductionism over holistic healing. In India, we treat the mind and body as one-smoking is a symptom, not a cause. To reduce a patient’s condition to enzyme kinetics is to ignore the spiritual and emotional roots of their illness. Perhaps if we addressed trauma instead of tweaking doses, we would not need such drastic interventions.
Chris Garcia
January 2, 2026 AT 04:39Ah, the beautiful dance of biochemistry and human will! CYP1A2, that quiet maestro of the hepatic orchestra, conducts its symphony with the smoke of rebellion, the steam of morning coffee, and the quiet sigh of a soul trying to breathe free. To reduce this to a dosage chart is to miss the poetry of survival-how the body, in its infinite wisdom, adapts, resists, and endures. Let us not forget: every molecule tells a story.
Kishor Raibole
January 2, 2026 AT 10:20Actually, this entire premise is flawed. In my clinical practice in Mumbai, we’ve observed that patients who smoke filtered cigarettes require lower doses than those who smoke bidis-contrary to the literature. The assumption that all tobacco smoke induces CYP1A2 equally is a colonial myth rooted in American studies. Our data suggests regional tobacco chemistry matters. Peer-reviewed? No. But real? Absolutely.
John Barron
January 3, 2026 AT 05:29Wait… so if I’m a smoker on clozapine and I drink 6 espressos a day, and then quit smoking and switch to decaf… I’m basically a walking time bomb? 😱 I’m not even kidding-I have a friend who just did this and now he’s on a feeding tube because he ‘felt fine.’ This is why I don’t trust doctors anymore. #PharmaLies
Gerald Tardif
January 4, 2026 AT 21:34Been there. My brother quit smoking after 20 years. We dropped his clozapine from 500mg to 350mg over 10 days, checked levels every 48 hours, and he’s been stable for 3 years now. No drama. Just science. And patience. You don’t have to be a genius-you just have to care enough to check.
Will Neitzer
January 6, 2026 AT 10:33Therapeutic drug monitoring is not merely a recommendation-it is the ethical imperative of modern psychopharmacology. To neglect TDM in clozapine management is not negligence; it is malpractice. The data is unequivocal. The guidelines are explicit. The consequences are irreversible. Let us not confuse convenience with competence.
Janice Holmes
January 6, 2026 AT 17:56So let me summarize: Smoke? Higher dose. Quit? Lower dose. Vape? Maybe higher, maybe lower, who knows? Coffee? Oh, and don’t forget that. Genetics? Irrelevant. TDM? Mandatory. And if you skip it? You’re basically signing someone’s death warrant. 🎉
Miriam Piro
January 7, 2026 AT 17:27It’s wild how the system ignores the obvious: if your body is literally burning through the drug because you’re smoking, then maybe the drug isn’t the problem-maybe the smoke is. But no, we’ll just keep dosing higher and higher… while the FDA sells you a $200 blood test every two weeks. 💸 It’s not medicine. It’s a money machine. And we’re all just pawns in it. 🕵️♀️
Alex Lopez
January 7, 2026 AT 20:48Let’s be real: the fact that this is even a debate is a tragedy. We have a drug with a narrow window, a known, massive interaction, and a simple fix: measure the blood. But we still rely on guesswork? That’s not clinical practice. That’s roulette with antipsychotics. I’ve seen people die because someone assumed they were ‘fine.’ Don’t be that person. Test. Adjust. Repeat. It’s not hard. It’s just necessary.