Diabetes Medications Safety Guide: Insulin and Oral Agents Explained
 Nov, 16 2025
Nov, 16 2025
Managing diabetes isn’t just about checking blood sugar-it’s about staying safe while doing it. Every day, millions of people take insulin or oral medications to control their blood glucose. But these lifesaving drugs can also be dangerous if used incorrectly. Hypoglycemia, kidney stress, infections, and even life-threatening ketoacidosis aren’t rare side effects-they’re real risks you need to understand before you take your next pill or injection.
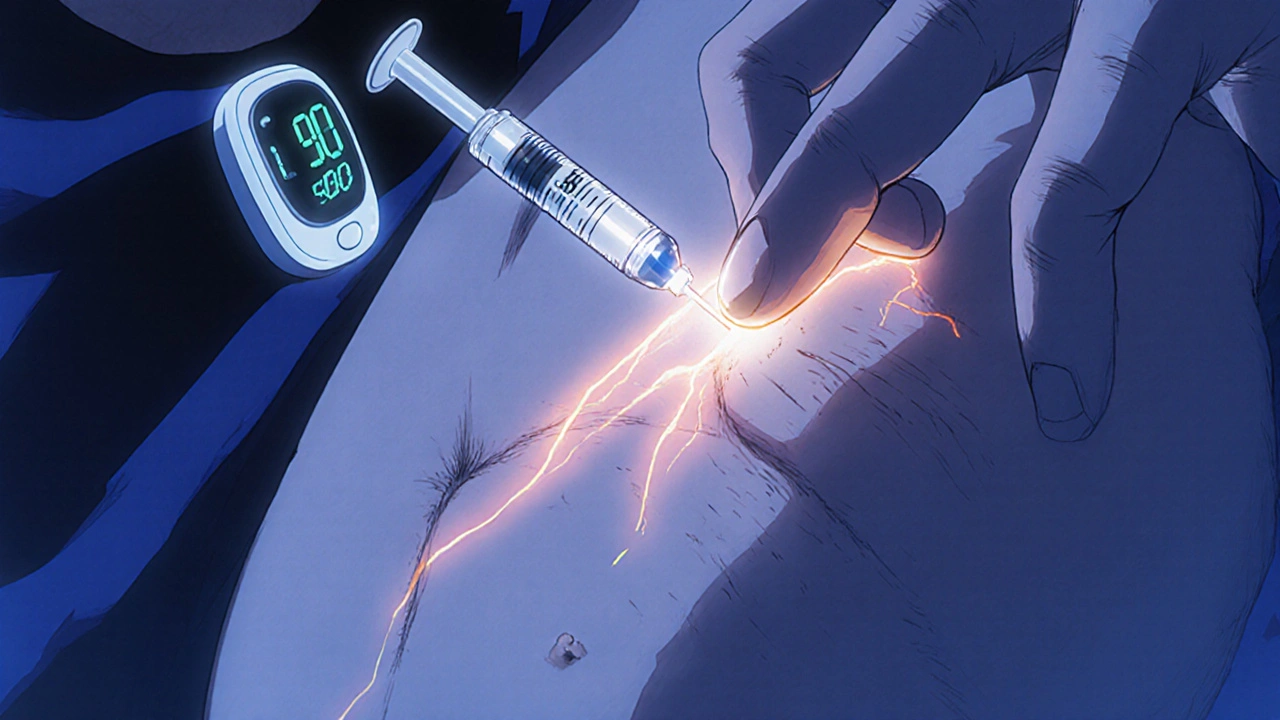
Insulin: Powerful, But Easy to Misuse
Insulin is the most effective tool for lowering blood sugar, especially for people with type 1 diabetes. But it’s also the most dangerous if dosed wrong. There are five main types: rapid-acting (like lispro), short-acting (regular insulin), intermediate (NPH), long-acting (glargine, degludec), and concentrated forms like Humulin R U-500. The U-500 version is five times stronger than standard insulin. If you mistake it for regular insulin, you could inject five times the dose-and end up in the hospital.
People often inject insulin into the same spot too often, leading to lumpy skin (lipohypertrophy). This messes with how fast the insulin is absorbed. One study found that patients who rotated injection sites had 30% fewer unpredictable blood sugar swings. Always use a new needle. Never reuse them. And never inject into muscle-always into fat tissue. Injecting into muscle can cause insulin to hit too fast, triggering sudden lows.
Automated insulin delivery (AID) systems, like hybrid closed-loop pumps, are changing safety. In clinical trials, these devices kept patients in their target blood sugar range 15% longer and cut severe hypoglycemia by nearly half compared to older pump systems. If you’re on insulin and still having frequent lows, talk to your doctor about switching to one.
Oral Medications: Not All Are Created Equal
There are ten types of oral diabetes pills, but only a few are used regularly. Metformin is still the first choice for type 2 diabetes. It’s safe for most people, doesn’t cause weight gain, and rarely causes low blood sugar. But it’s not for everyone. If your kidney function drops below an eGFR of 30, you must stop it. Between 30 and 45, use it with caution. Between 45 and 60, cut your dose in half. Many doctors skip checking kidney function before prescribing it-but that’s a mistake. Lactic acidosis, while rare, can be fatal if metformin builds up in your system due to poor kidney clearance.
Sulfonylureas like glipizide, glyburide, and glimepiride are older pills that force your pancreas to make more insulin. They’re cheap and effective-but they’re also the leading cause of dangerous hypoglycemia among oral drugs. Up to 40% of people on these meds have low blood sugar episodes. One in five of those are severe enough to need help from someone else. Older adults are especially at risk. A 70-year-old on glyburide might not feel their blood sugar drop until they’re dizzy, confused, or about to fall. That’s why experts recommend avoiding glyburide in seniors. Glipizide is safer because it’s cleared by the liver, not the kidneys.
Newer Drugs: Benefits with Hidden Risks
Medications like SGLT2 inhibitors (empagliflozin, dapagliflozin) and GLP-1 agonists (semaglutide, liraglutide) are popular now because they protect the heart and kidneys. But they come with new dangers. SGLT2 inhibitors can cause diabetic ketoacidosis-even when your blood sugar isn’t high. This is called euglycemic DKA. It’s rare, but it’s real. Over 5% of all DKA cases linked to these drugs happen with blood sugar under 250 mg/dL. That means you might feel awful-nausea, vomiting, stomach pain-but your glucometer looks fine. If you’re on one of these drugs and feel sick, test for ketones with a urine strip or blood meter. Don’t wait for high sugar to panic.
These drugs also cause genital yeast infections in about 4-5% of users. It’s more common in women, but men get them too. If you notice itching, redness, or discomfort down there, don’t ignore it. It’s not embarrassing-it’s a side effect. And it’s treatable.
GLP-1 agonists like Ozempic and Mounjaro cause nausea and vomiting in up to half of users, especially at first. Many people quit because of it. The trick? Start low. Go slow. Your body adjusts. Never increase the dose faster than your doctor says. And never take them if you have a history of pancreatitis.
Drug Interactions: The Silent Danger
Diabetes meds don’t live in a vacuum. They mix with other drugs you take-and that’s where things go wrong. Antibiotics like Bactrim (sulfamethoxazole/trimethoprim) can boost insulin’s effect and send your blood sugar crashing. Beta-blockers hide the warning signs of low blood sugar-like shaking and fast heartbeat-so you don’t feel it coming. Some antidepressants, statins, and even common painkillers like NSAIDs can interfere with glucose control.
If you’re starting a new medication-even something as simple as an OTC cold pill-ask your pharmacist: “Will this affect my diabetes drugs?” Don’t assume it’s safe. Many people don’t realize that herbal supplements like bitter melon or cinnamon can also lower blood sugar. Taken with metformin or insulin? That’s a recipe for a low.
Special Populations: Seniors, Kidneys, and Surgery
If you’re over 65, your body handles drugs differently. Your kidneys slow down. Your liver processes things slower. Your brain becomes less sensitive to low blood sugar. That’s why doctors should start older adults on lower doses of sulfonylureas and insulin. Tight blood sugar goals? Not worth the risk. A1c of 7.5% is safer than 6.5% for seniors. Falling from a low is more dangerous than a slightly higher number.
Kidney problems change everything. SGLT2 inhibitors are off-limits if you’re on dialysis. Metformin needs dose cuts as kidney function drops. Even insulin may need adjustment because your body clears it slower. Always get an eGFR test before starting any new diabetes drug-and repeat it yearly.
Before any surgery-even a dental extraction-stop SGLT2 inhibitors at least 24 hours ahead. This cuts DKA risk by over 90%. If you’re on insulin, your care team should give you a special plan for the day of surgery. Don’t skip this step. A routine procedure can turn deadly if your meds aren’t managed properly.

What You Can Do Today
Safety isn’t just your doctor’s job. It’s yours too. Here’s what to do right now:
- Keep a written log: What you take, when, and any side effects. Use your phone if you prefer.
- Know your kidney number (eGFR). Ask for it at your next checkup.
- Check your injection sites. Are they lumpy? Rotate them weekly.
- Test for ketones if you’re sick, stressed, or on an SGLT2 inhibitor and feel unwell-even if your sugar is normal.
- Never skip meals if you’re on sulfonylureas or insulin. Carry fast-acting sugar (glucose tabs, juice) with you.
- Wear a medical ID bracelet. It could save your life if you pass out.
- Ask your pharmacist to review all your meds every six months. They catch interactions your doctor might miss.
Technology helps. Continuous glucose monitors (CGMs) show trends, not just snapshots. They alert you to lows before they happen-even at night. If you’re still using fingersticks only, talk to your doctor about upgrading. Most insurance covers them now.
When to Call for Help
You don’t need to guess when something’s wrong. Call your doctor or go to urgent care if you have:
- Confusion, dizziness, or trouble speaking
- Severe nausea or vomiting with abdominal pain
- Unexplained fatigue or rapid breathing
- Low blood sugar that won’t rise after treatment
- Any new rash, swelling, or breathing trouble after starting a new drug
These aren’t normal side effects. They’re red flags. Don’t wait. Don’t hope it passes. Act fast.
Diabetes meds are tools. They’re not magic. They work best when you know how to use them safely-and when you know what to watch for. The goal isn’t just to control sugar. It’s to live without fear of the next low, the next infection, the next hospital visit. Stay informed. Stay vigilant. And never stop asking questions.
Can I stop my diabetes medication if my blood sugar is normal?
No. Normal blood sugar doesn’t mean your diabetes is cured. Stopping insulin or oral meds without medical supervision can cause your sugar to spike dangerously fast, especially with type 1 diabetes. Even if you’ve lost weight or improved your diet, your body may still need medication to stay in range. Always talk to your doctor before making changes.
Which diabetes drug has the lowest risk of low blood sugar?
Metformin, DPP-4 inhibitors (like sitagliptin), and GLP-1 receptor agonists (like semaglutide) have the lowest risk of hypoglycemia when used alone. SGLT2 inhibitors also carry low hypoglycemia risk unless combined with insulin or sulfonylureas. Sulfonylureas and insulin are the highest risk. Always ask your doctor which drug fits your personal safety profile.
Why do SGLT2 inhibitors cause yeast infections?
SGLT2 inhibitors make your kidneys dump sugar into your urine. That sugar feeds yeast, especially in warm, moist areas like the genitals. It’s not an infection from poor hygiene-it’s a direct side effect of how the drug works. About 4-5% of users get it. It’s treatable with antifungal creams or pills, and often goes away after a few weeks. If it keeps coming back, talk to your doctor about switching.
Is it safe to drink alcohol while on diabetes meds?
It’s risky. Alcohol can block your liver from releasing glucose, which increases hypoglycemia risk-especially with insulin or sulfonylureas. The danger is worse if you drink on an empty stomach or after exercise. If you drink, always eat something, limit yourself to one drink, and check your blood sugar before bed. Avoid alcohol entirely if you’re on an SGLT2 inhibitor-it raises your risk of ketoacidosis.
What should I do if I miss a dose of my diabetes medication?
It depends on the drug. For metformin, take it as soon as you remember-if it’s not close to your next dose. For insulin, never double up. Call your doctor for advice. For sulfonylureas, if you miss a dose before a meal, skip it-don’t take it later. For SGLT2 inhibitors, take it as soon as you remember, but skip it if it’s already the next day. Always check your medication guide or ask your pharmacist. Guessing can be dangerous.
If you’re taking multiple medications, consider asking for a Collaborative Drug Therapy Management (CDTM) plan. This means your pharmacist, doctor, and nurse work together to spot conflicts before they hurt you. It’s not common everywhere-but it’s one of the most effective ways to avoid preventable hospital visits.
Diabetes care has come a long way since insulin was first discovered in 1922. But safety hasn’t kept pace with innovation. New drugs bring new risks. The best way to protect yourself is to know your meds, know your body, and never be afraid to speak up.

kora ortiz
November 18, 2025 AT 11:20Just started using a CGM last month and my life changed. No more midnight panic attacks over low blood sugar. I used to wake up sweaty and shaking, now I get a gentle alert and sip some juice while still half-asleep. This post nailed it-technology isn’t magic, but it’s the closest thing we’ve got to a safety net.
Jeremy Hernandez
November 20, 2025 AT 04:00Anyone else think Big Pharma just invented all these new drugs so they can sell us ketone strips and antifungal cream on top of our insulin bills? SGLT2 inhibitors cause yeast infections? Wow. Groundbreaking. Next they’ll tell us sugar in urine attracts ants. Meanwhile, my grandpa’s on glyburide and still drives his tractor at 78. Maybe we should stop over-medicalizing everything.
henry mariono
November 22, 2025 AT 01:32Thanks for the detailed breakdown. I’ve been avoiding talking to my doctor about my injection sites because I didn’t realize lumps could affect absorption. Going to check them this weekend. Small step, but it matters.
Joseph Peel
November 22, 2025 AT 19:24The point about pharmacist medication reviews cannot be overstated. I had a patient on metformin and Bactrim who developed lactic acidosis. The antibiotic interaction was never flagged. Pharmacists are the last line of defense. Advocate for that review-it’s not extra, it’s essential.
Kelsey Robertson
November 22, 2025 AT 20:45Wait-so we’re supposed to believe that ‘euglycemic DKA’ is a real thing? That’s not a medical condition-it’s a marketing term invented so drug companies can scare you into buying ketone strips every month. And ‘rotate injection sites’? Please. My cousin’s been injecting in the same spot for 12 years and he’s fine. Maybe your body adapts, instead of your doctor panicking?
Joseph Townsend
November 23, 2025 AT 05:40Let’s be real-this whole diabetes industrial complex is a circus. You got your insulin, your pumps, your CGMs, your ketone strips, your antifungal creams, your ‘don’t drink alcohol unless you’re holding a juice box’ rules… I’m starting to think diabetes isn’t a disease-it’s a subscription service. I’m just waiting for the ‘Diabetes Lifestyle NFT’ to drop.
Bill Machi
November 23, 2025 AT 20:19As an American veteran who’s seen too many VA patients die from mismanaged diabetes, I can tell you this: the real danger isn’t the drugs-it’s the incompetence. Doctors who don’t check eGFR. Pharmacies that don’t warn about interactions. Patients who skip meals because they’re ‘trying to lose weight.’ This isn’t about innovation-it’s about basic competence. And if you’re not demanding it, you’re part of the problem.
Elia DOnald Maluleke
November 24, 2025 AT 22:31In my village in South Africa, we use bitter melon tea and exercise to manage sugar. We do not have access to CGMs or GLP-1 agonists. Yet, our elders live long, quiet lives. Perhaps the real issue is not the medication-but the belief that every problem requires a pharmaceutical solution. Simplicity, patience, and community care have value too.
satya pradeep
November 25, 2025 AT 11:39Bro, I’m on metformin and started taking cinnamon capsules ‘for extra help’-ended up in ER with a sugar of 42. Never again. Always talk to your doc before adding ‘natural’ stuff. Seriously. It’s not safer just because it’s from a tree.