Double-Checking Medication Strength and Quantity Before Leaving the Pharmacy
 Dec, 8 2025
Dec, 8 2025
Imagine this: you pick up your child’s antibiotic prescription. The pharmacist hands you a bottle. You read the label: 5 mL. You give it to your kid using the plastic spoon that came with it. A few hours later, your child is vomiting, lethargic, and in the ER. Turns out, the prescription was for 0.5 mL - not 5 mL. The pharmacy gave you the right medicine, but the wrong amount. And no one caught it.
This isn’t a rare horror story. It happens more often than you think. And the fix? Simple. But only if you do it right.
Why Double-Checking Medication Strength and Quantity Matters
Medication errors kill over 250,000 people in the U.S. every year. About 63% of those fatal errors involve high-risk drugs like insulin, blood thinners, or opioids. And a huge chunk of those mistakes? They happen because someone didn’t double-check the strength and total quantity before handing over the bottle.
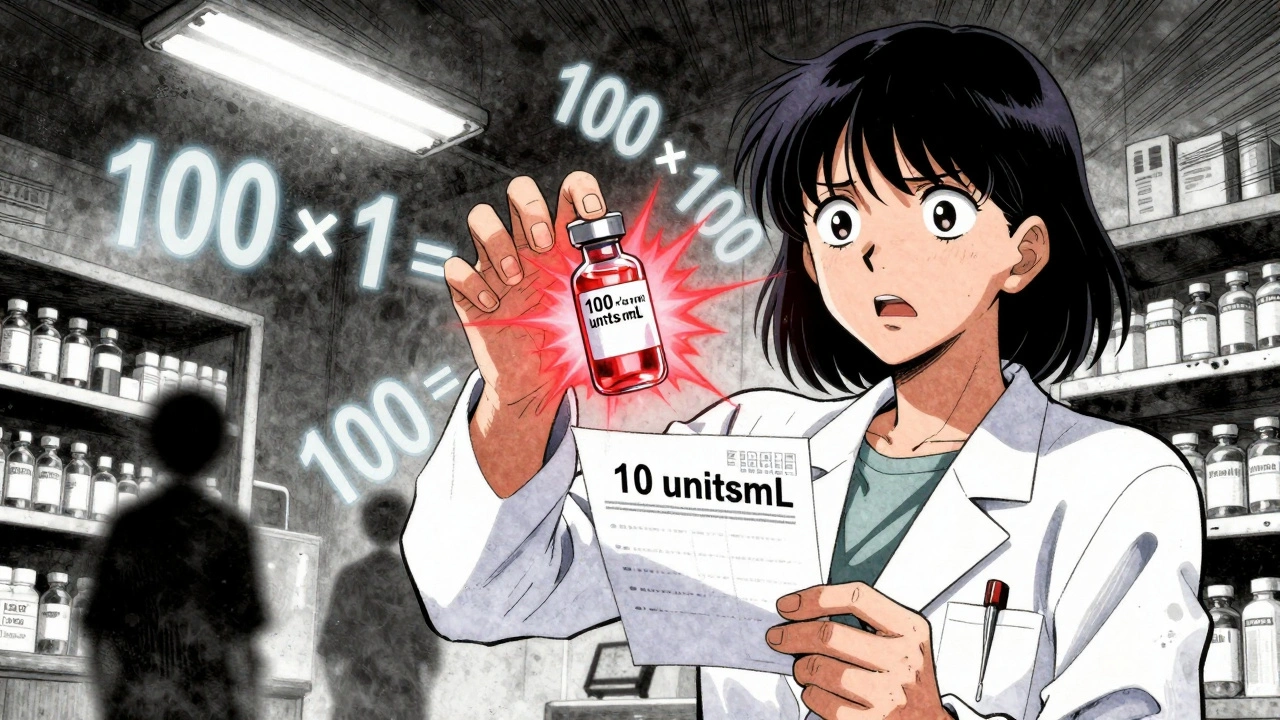
Strength means how much drug is in each unit - like 10 mg per tablet or 5 mg per mL. Quantity is the total amount in the container - like 30 tablets or 100 mL. Mixing those up can be deadly. A parent might think a 10 mL bottle contains 10 mg total. But if it’s labeled 1 mg/mL, that’s actually 10 mg total - not 1 mg. That’s a tenfold error. And it’s happened. More than once.
The Institute for Safe Medication Practices (ISMP) calls this the most critical safety step in community pharmacy. They say if you do nothing else, verify strength and quantity before the patient walks out. The Agency for Healthcare Research and Quality (AHRQ) found this single step prevents 87% of strength-related dispensing errors.
How to Double-Check Like a Pro
It’s not enough to glance at the label. You need a system.
- Read the prescription first. What did the doctor order? 5 mg/mL? 100 mL total? Write it down.
- Check the bottle label. Is the strength listed as per mL or total amount? The FDA says the total amount must be the most prominent number on the label - bigger font, clearer placement. If it’s not, that’s a red flag.
- Recalculate it. If the bottle says 2 mg/mL and contains 50 mL, the total drug is 100 mg. Multiply it. Don’t assume. Do the math. Even if you’ve done it a thousand times.
- Compare to the original order. Did the system print 50 mL but the script said 30? Did the strength change from 1 mg/mL to 2 mg/mL without a new signature? Stop. Call the prescriber.
- Verify the dosing device. If it’s a liquid, did you give them a calibrated oral syringe? Not a teaspoon? Not a kitchen spoon? Household spoons vary wildly - one can hold 3 mL, another 10 mL. The FDA says this causes 93% of pediatric dosing errors.
One pharmacist in Ohio caught a fatal insulin error because she recalculated. The script said 10 units/mL. The vial said 100 units/mL. The technician had grabbed the wrong vial. The math didn’t add up. She stopped it. The patient didn’t get a lethal dose.
What Happens When You Skip This Step
There’s a Reddit thread from a pharmacy tech who admitted he skipped double-checks during a staffing crunch. He dispensed 10 times the levothyroxine dose. The patient ended up in cardiac arrest. Survived. But lost her job. And her peace of mind.
Another case: a 78-year-old woman got 5 mL of liquid morphine instead of 0.5 mL. She was found unconscious at home. The pharmacy had given her a kitchen teaspoon. The label said 1 mg/mL. She thought 5 mL meant 5 mg - not 5 mg total. She got 5 mg. But the prescription was for 0.5 mg. She was 10 times over. She survived. But barely.
These aren’t anomalies. They’re patterns. The Joint Commission reports that 68% of medication-related sentinel events from 2020 to 2022 involved incorrect strength or quantity. And pediatric cases make up 41% of those.
Technology Helps - But Doesn’t Replace Human Judgment
Barcode scanning cuts dispensing errors by 83%. Electronic prescriptions that auto-calculate total dose? Great. But they’re not foolproof.
One pharmacy in Florida had barcode scanners. Still, a tech scanned the wrong vial. The system didn’t flag it because the barcode was valid - just the wrong product. The tech didn’t look at the label. Didn’t recalculate. The patient got 10 times the dose.
Technology is a tool. Not a replacement for your eyes, your brain, and your responsibility.
Even the best system can fail. But a trained human who double-checks? That’s the last line of defense.
The Real Barrier: Time and Pressure
Most pharmacists and techs know they should double-check. The problem? They’re rushed.
Corporate chains push for 35+ prescriptions per hour. That’s less than 2 minutes per script. But a real double-check - recalculating, verifying the device, reading the label - takes 45 to 60 seconds. Alone. No distractions.
On AllNurses.com, 73% of pharmacy techs say they feel pressured to skip steps during peak hours - 7 to 10 a.m. and 4 to 7 p.m. That’s when most errors happen.
Independent pharmacies are worse off. 68% with fewer than five staff report inconsistent double-checking. No backup. No time. No safety net.
But here’s the truth: skipping a double-check to save 30 seconds doesn’t save time. It creates a hospital visit. A lawsuit. A loss of license. A broken family.

What You Can Do - Even If You’re Not a Pharmacist
You don’t have to be a professional to protect yourself or your loved ones.
- Ask: “Is this the total amount?” If the label says 5 mg/mL and you have 100 mL, ask: “So the bottle has 500 mg total?” If they hesitate, pause.
- Ask for the right tool. Never accept a teaspoon. Always ask for an oral syringe - especially for kids. They cost less than a dollar. Pharmacies should give them for free.
- Check the numbers yourself. If it’s a liquid, multiply the strength by the volume. 2 mg/mL × 30 mL = 60 mg total. Does that match what the doctor ordered?
- Don’t assume. If the label looks different from last time - even slightly - ask. That’s how errors sneak in.
One mother told ISMP she saved her son’s life by asking, “Is this 0.5 mL or 5 mL?” The pharmacist paused. Looked. Realized he’d grabbed the wrong bottle. He apologized. She didn’t leave angry. She left safe.
The Future Is Clear - But the Responsibility Is Now
The FDA is pushing new rules: by 2025, all injectable medications must display the total amount in bold, oversized font. USP is working on digital verification systems that auto-check strength against national databases.
But none of that matters if the person handing you the bottle doesn’t look at it.
Double-checking isn’t bureaucracy. It’s not paperwork. It’s the moment between a mistake and a tragedy.
It’s the difference between a child going to school tomorrow - or ending up in intensive care.
It’s the difference between a senior living at home - or dying from a simple math error.
So before you leave the pharmacy - pause. Look. Ask. Confirm.
Because the bottle you’re holding? It’s not just medicine. It’s a promise. And someone’s life depends on you making sure it’s kept.

Katie Harrison
December 9, 2025 AT 23:17I’ve been a pharmacist for 18 years, and I still double-check every liquid med with the script in hand-no exceptions. One time, I caught a 10x insulin error because I multiplied the mL and the concentration. I didn’t trust the system. I trusted my brain. And I’ll keep doing it, even when the line’s out the door.
Mona Schmidt
December 11, 2025 AT 19:37There’s a quiet dignity in pausing to verify. It’s not about being slow-it’s about being responsible. In Canada, we don’t have the same corporate pressure, but we still see mistakes. I always ask for the syringe. Always. Because my niece almost didn’t make it through her first antibiotic course because of a kitchen spoon.
Michael Robinson
December 12, 2025 AT 02:29Life’s simple sometimes. You don’t need fancy tech. You just need to look. And think. And care. That’s it. The rest is noise.
Kathy Haverly
December 13, 2025 AT 21:16Oh great, another guilt-trip post. So now I’m supposed to feel like a monster because I didn’t recalculate the dose on my 7-year-old’s amoxicillin? Newsflash: I’m not a pharmacist. I’m a single mom who works two jobs. You want me to stop and do math in a 45-minute pharmacy line? Try living my life before you preach.
Suzanne Johnston
December 15, 2025 AT 11:10There’s a tension here between human care and systemic failure. The pharmacist who caught the insulin error? She was doing her job. But why should one person’s vigilance be the only thing standing between a child and death? We need systems that protect us from our exhaustion, not just ask us to be heroes.
Haley P Law
December 16, 2025 AT 06:20OMG I JUST HAD THIS HAPPEN 😭 I took my son’s medicine home and the bottle said 5ml and I thought it was 5mg… I almost gave him the whole thing. I was about to pour it in his mouth when I saw the tiny "per mL" on the label. I screamed. My husband thought I was having a seizure. I called the pharmacy. They apologized. I cried for an hour. Please. Just… please double-check. I can’t do this again.
Andrea DeWinter
December 16, 2025 AT 23:32Always use the syringe. Always. Even if they say "it’s fine". Even if you’re in a hurry. Even if it’s your third script today. I’ve seen too many kids end up in the ER because someone used a teaspoon. Pharmacies should hand them out like gum. They cost pennies. The ER visit costs thousands. Don’t be cheap with safety.
Steve Sullivan
December 17, 2025 AT 02:50man i used to think this was overkill til my cousin got the wrong dose of his seizure med. he was fine but the pharmacy didn’t even notice they gave him 10x. i just stared at the label and went "wait… that’s not right". turns out the tech scanned the wrong bottle and the system didn’t catch it. now i always multiply the numbers. no shame in doing the math. better safe than sorry.
George Taylor
December 17, 2025 AT 07:19...And yet, despite all this, the FDA still allows pharmacies to print "Total Volume: 100 mL" in 8pt font, while "1 mg/mL" is in 12pt bold. The system is designed to fail. The fact that you’re even reading this means you’re already part of the problem-you’re the one who’s supposed to catch it. Not the pharmacist. Not the tech. You. And that’s not safety. That’s exploitation.