Genetic Factors in Statin Tolerance: How Pharmacogenomics Testing Can Help
 Jan, 13 2026
Jan, 13 2026
Statin Tolerance Calculator
Your Genetic Profile
Based on the SLCO1B1 gene variant, this tool helps identify which statins are safest for you.
For millions of people taking statins to lower cholesterol and prevent heart attacks, the biggest problem isn’t the medication itself-it’s the muscle pain that makes them quit. Up to 29% of users report muscle aches, weakness, or cramps so severe they stop taking their pills. And here’s the twist: it’s not always about dosage, age, or exercise. For many, the real culprit is hidden in their DNA.
Why Some People Can’t Tolerate Statins
Statins work by blocking an enzyme your liver uses to make cholesterol. But they don’t just stay in the liver. Some of the drug leaks into your bloodstream and ends up in your muscles. That’s where trouble starts. Muscle cells don’t handle statins well, and for some people, even low doses cause pain. But why do some people react badly while others feel fine? The answer lies in a gene called SLCO1B1 a gene that codes for a protein responsible for moving statins from the blood into the liver. If your version of this gene has a specific mutation-called c.521T>C or rs4149056-your liver can’t grab statins as quickly. That means more of the drug hangs around in your muscles, causing damage. This isn’t rare. About 15% of people of European descent carry one copy of this variant, and 1-2% carry two copies. Those with two copies are nearly five times more likely to develop severe muscle injury on high-dose simvastatin.Which Statins Are Affected-and Which Aren’t
Not all statins are created equal when it comes to genetics. The SLCO1B1 gene issue hits simvastatin hardest. That’s why clinical guidelines specifically warn against giving 80mg simvastatin to people with the CC genotype. But switch to atorvastatin or rosuvastatin, and the risk drops dramatically. A 2021 study of nearly 12,000 patients found no link between SLCO1B1 and muscle symptoms with these two statins. Why? Because atorvastatin and rosuvastatin use different transporters to enter the liver. They don’t rely as much on the OATP1B1 protein that SLCO1B1 makes. That’s why switching from simvastatin to pravastatin or fluvastatin often solves the problem. One woman in her 50s, after three failed attempts with simvastatin, switched to pravastatin following genetic testing. Her LDL dropped from 168 to 92 mg/dL-and her muscle pain vanished. She’s been on it for over a year with no issues.Other Genes That Might Play a Role
SLCO1B1 is the star of the show, but it’s not the only player. Other genes like CYP2D6, CYP3A4, and ABCB1 affect how your body breaks down or flushes out statins. About 7-10% of people have slow versions of CYP2D6, which can cause statins to build up in the blood. Then there’s GATM and CACNA1S, genes involved in muscle energy and calcium flow. A 2021 study found a strong signal in the SOAT1 gene, which handles cholesterol storage in cells-but we still don’t know exactly how it causes muscle pain. The problem? Most of these genes only explain a tiny part of the risk. SLCO1B1 accounts for about 6% of statin-related muscle symptoms. That means even if you test negative for the variant, you could still get muscle pain. Genetics is just one piece of the puzzle. Age, kidney function, thyroid issues, and even vitamin D levels matter too.Who Should Get Tested-and When
Right now, testing isn’t for everyone. The Clinical Pharmacogenetics Implementation Consortium (CPIC) a group of experts that creates guidelines for using genetic test results in prescribing says testing is most useful if you’ve already had muscle symptoms on a statin and want to try again. It’s also recommended before starting high-dose simvastatin if you’re at high risk for heart disease but have a history of muscle pain with other drugs. Testing before your first statin-called pre-emptive testing-is gaining traction. A 2021 study showed that people who got tested before starting statins were 18.7% more likely to stick with them long-term. That’s huge. If you’re on a statin now and feeling off, testing can help you find a version that works. If you’ve never taken one but have a family history of statin intolerance, it might be worth asking your doctor.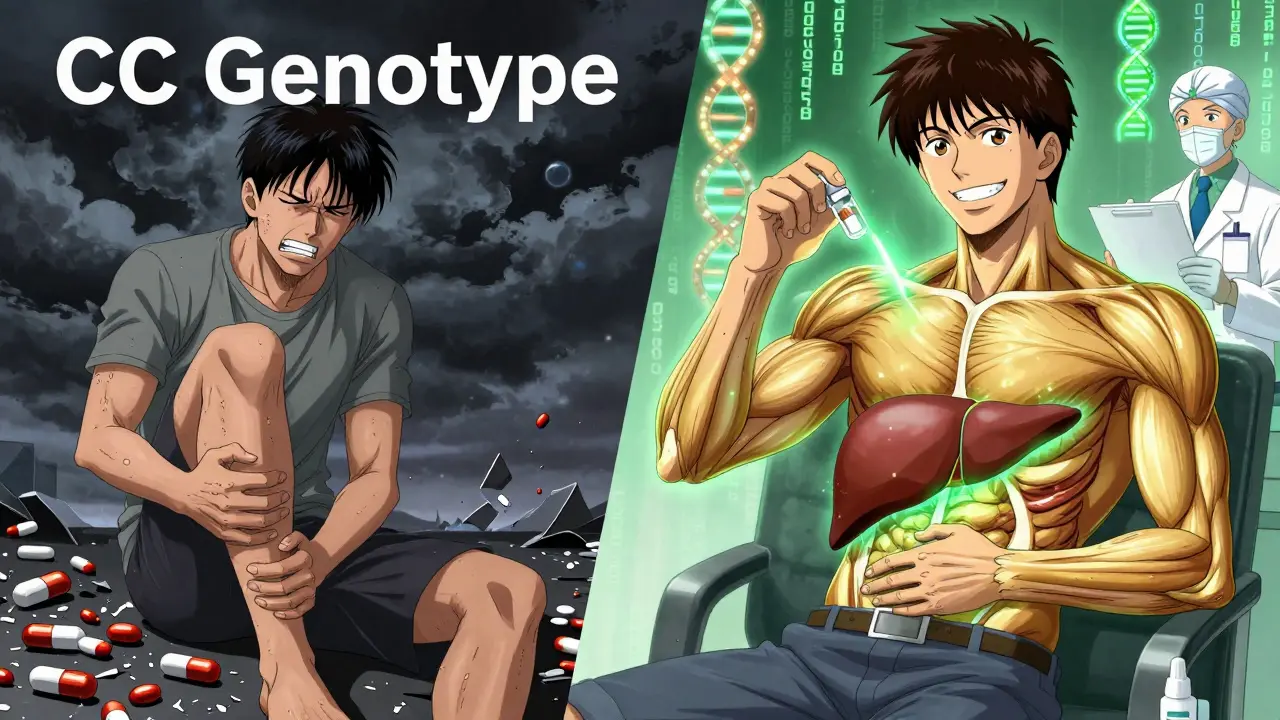
How the Test Works and What It Costs
Getting tested is simple. Most labs use a cheek swab-you rub a small brush inside your mouth, mail it in, and wait 5-10 days. Blood samples work too. The test looks for the SLCO1B1 variant and sometimes includes CYP2D6 and ABCB1. Companies like Mayo Clinic Laboratories, ARUP Laboratories, and Color Genomics offer these tests. Costs vary. Standalone SLCO1B1 testing runs $150-$400 out of pocket. Insurance coverage is spotty. As of 2022, only 28% of commercial insurers paid for it. Medicare rarely covers it unless it’s part of a larger pharmacogenomic panel tied to a specific clinical situation. Some employers and health systems offer it as part of wellness programs, especially if you’re already getting other genetic screenings.What Your Results Mean
Your report will likely say one of three things:- TT-normal function. You’re at lowest risk for muscle injury on simvastatin.
- TC-one copy of the variant. Moderate risk. Avoid high-dose simvastatin (80mg). Lower doses (20-40mg) are usually fine.
- CC-two copies. High risk. Don’t take simvastatin 80mg. Even lower doses carry increased risk. Switch to atorvastatin, rosuvastatin, or pravastatin.
Why Some Doctors Are Still Skeptical
Despite strong evidence, not everyone is convinced. A 2020 randomized trial published in JAMA Network Open gave SLCO1B1 results to doctors treating patients with prior statin intolerance. The result? No big change in muscle symptoms or adherence. Patients still stopped taking their meds at the same rate. Why? Because genetics isn’t the whole story. Some people feel muscle pain even with low-risk genotypes. Others feel fine despite having the high-risk variant. And if your doctor doesn’t know what to do with the result, the test doesn’t help. The American College of Cardiology a leading authority on heart disease guidelines says testing “may be considered” after intolerance-but doesn’t recommend it for everyone. They’re waiting for proof that testing improves long-term heart outcomes. Right now, we know it helps people stay on statins. We don’t yet know if that translates to fewer heart attacks.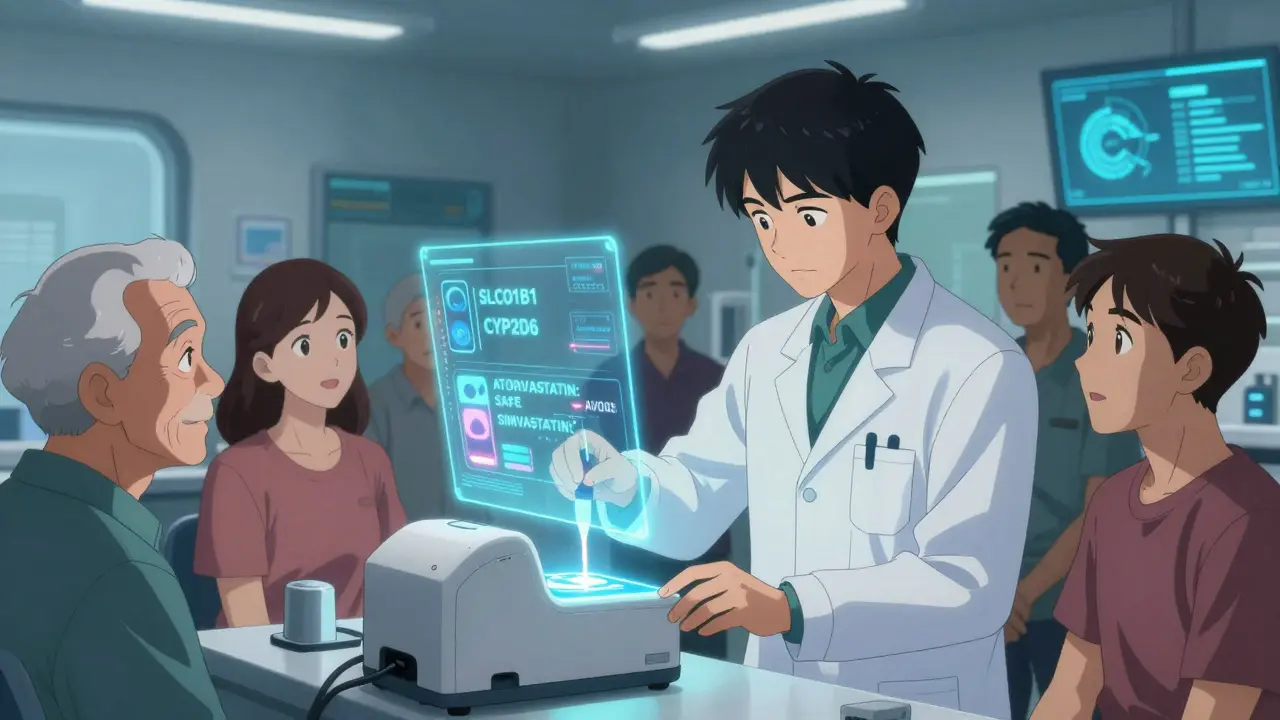
What’s Next for Pharmacogenomics and Statins
The future isn’t just about one gene. Researchers are building polygenic risk scores-combining SLCO1B1 with 10-15 other variants to predict risk more accurately. Early results show these scores improve prediction from 58% to 67% accuracy. That’s still not perfect, but it’s progress. A new group called the Statin Pharmacogenomics Implementation Consortium a multi-institutional effort to standardize genetic testing for statins across U.S. hospitals is working to roll out testing in 50 health systems by 2025. They’re creating templates for lab reports, training tools for doctors, and protocols for EHR integration. Meanwhile, the market is growing fast. The global pharmacogenomics market is expected to hit $21 billion by 2030. Statin testing makes up a third of that. As costs drop and insurance coverage improves, this could become routine.Real Stories, Real Choices
On Reddit, a 2022 thread with over 140 comments showed that 62% of people who got tested and switched statins based on results felt better. But 38% said it made no difference. One man wrote: “I had the CC genotype. My doctor told me to avoid simvastatin. I switched to rosuvastatin. No more pain. My cholesterol’s down. I finally feel like I’m in control.” Another said: “I tested negative. Still got muscle pain. Stopped everything. Now I take ezetimibe instead.” The takeaway? Genetics can guide you-but it doesn’t dictate your fate. If you’ve quit statins because of muscle pain, don’t give up on treatment. Talk to your doctor about testing. Ask if switching statins is an option. Ask if your pharmacy has a pharmacogenomics specialist. You might find a version that works.What You Can Do Today
If you’re on a statin and experiencing muscle pain:- Don’t stop cold turkey-talk to your doctor first.
- Ask if your current statin is simvastatin. If yes, ask if switching to atorvastatin or rosuvastatin is possible.
- Request a pharmacogenomics test for SLCO1B1, especially if you’ve had muscle pain before.
- If your doctor says no, ask for a referral to a cardiologist or clinical pharmacist who understands pharmacogenomics.
- Check if your health system offers pre-emptive testing as part of a wellness program.
Is pharmacogenomics testing for statins covered by insurance?
Insurance coverage is inconsistent. As of 2023, only about 28% of commercial insurers cover SLCO1B1 testing. Medicare rarely covers it unless it’s part of a broader pharmacogenomic panel tied to a specific medical need. Out-of-pocket costs range from $150 to $400. Some employers, academic hospitals, and health systems offer testing for free as part of research or wellness programs.
Can I get tested before starting a statin?
Yes. Pre-emptive testing-done before you start any statin-is becoming more common, especially in larger health systems. Studies show it improves long-term adherence by nearly 20%. If you have a family history of statin intolerance or are at high risk for heart disease, asking for testing upfront can save you from months of trial and error.
Does SLCO1B1 testing work for all statins?
No. The SLCO1B1 variant strongly affects simvastatin, but has little to no impact on atorvastatin, rosuvastatin, pravastatin, or fluvastatin. That’s why guidelines only recommend testing for simvastatin. If you’re on another statin and still have muscle pain, the cause is likely something else-like age, thyroid issues, or another gene.
If I test positive, do I have to avoid statins forever?
No. You just need to avoid high-dose simvastatin. Many people with the CC genotype tolerate low-dose simvastatin (10-20mg) or switch to atorvastatin, rosuvastatin, or pravastatin without issues. The goal isn’t to avoid statins-it’s to find the right one for your genes.
Are there alternatives if I can’t take any statin?
Yes. Ezetimibe, PCSK9 inhibitors (like evolocumab), and bempedoic acid are non-statin options that lower LDL cholesterol. They don’t cause muscle pain the same way statins do. But they’re more expensive and often reserved for people who truly can’t tolerate statins. Genetic testing can help you avoid unnecessary use of these drugs by finding a statin that works.

Lance Nickie
January 15, 2026 AT 09:30statins are just fancy placebos with side effects. my buddy took one and his legs turned to jelly. no gene test needed.
Milla Masliy
January 16, 2026 AT 00:01My mom switched from simvastatin to pravastatin after genetic testing and hasn’t had a single muscle cramp since. She’s 72 and more active than I am. It’s not magic-it’s science. If your doctor won’t order the test, ask for a pharmacist who knows pharmacogenomics. Seriously, it’s life-changing.
Angel Molano
January 17, 2026 AT 17:31Stop wasting money on genetic tests. People just want an excuse to quit their meds. Muscle pain? Maybe you’re not exercising or eating right. Blaming DNA is lazy.
Vinaypriy Wane
January 18, 2026 AT 17:36I’ve been on atorvastatin for five years-zero pain. But my cousin, same age, same weight, took simvastatin and couldn’t walk. She got tested, found out she was CC… and switched. Now she’s fine. Genetics isn’t destiny-it’s a map. Use it.
Diana Campos Ortiz
January 20, 2026 AT 15:25i’ve had muscle pain on every statin i’ve tried… even rosuvastatin. tested negative for slco1b1. so… what now? just take ezetimibe and hope? feels like the system gives you a checklist but no real answers.
Jesse Ibarra
January 21, 2026 AT 08:26Of course the pharmaceutical industry loves this. More tests. More data. More $$$ for labs. Meanwhile, people are dying from untreated high cholesterol because they’re too busy swabbing their cheeks to actually take a pill. This isn’t medicine-it’s tech bro nonsense wrapped in a lab coat.
Randall Little
January 23, 2026 AT 01:27So let me get this straight: we’re spending $400 to find out we can’t take simvastatin… but the solution is just to take a different statin that costs 3x as much? And you’re calling this progress? I’d rather just eat more fiber and hope for the best.
Acacia Hendrix
January 24, 2026 AT 00:23It’s fascinating how the SLCO1B1 variant modulates hepatic uptake kinetics via the OATP1B1 transporter, yet the clinical utility remains attenuated by polygenic and epigenetic confounders. The 6% variance explained is statistically significant but clinically insufficient-especially when CYP2D6 phenotyping and ABCB1 haplotype analysis are rarely integrated. We’re treating a multivariate problem with a univariate solution. It’s like diagnosing hypertension with a single blood pressure reading.
James Castner
January 24, 2026 AT 19:45Let’s not lose sight of the bigger picture: we’re not just talking about genes or drugs-we’re talking about human dignity. For years, people were told their pain was "all in their head," or that they were "non-compliant." Now, science says: no, your body is literally telling you something your doctor didn’t know how to hear. This isn’t about cost or convenience. It’s about listening. It’s about humility. It’s about recognizing that biology doesn’t care about your insurance plan, your doctor’s schedule, or your reluctance to learn. The data is here. The tools exist. The only thing missing is the will to use them. We owe it to every person who’s quit their statin in despair to make this accessible-not just for the wealthy, not just for the well-connected, but for everyone. This is medicine becoming human.
Adam Rivera
January 25, 2026 AT 17:31My uncle got tested after he couldn’t take any statin. Switched to pravastatin. LDL dropped from 190 to 88. No pain. He’s hiking in Colorado now. Just wanted to say: if you’re struggling, don’t give up. There’s probably a version that works for you. Ask your doc. Or better yet, ask the pharmacy.
John Tran
January 26, 2026 AT 11:39you know what’s wild? we’ve been treating cholesterol like it’s a villain… but what if it’s just doing its job? maybe the real problem is that we’re forcing our bodies to adapt to a diet and lifestyle that evolved over 10,000 years in 20 years? i mean… we’re basically asking our cells to run a marathon on a treadmill made of donuts. and then we blame the genes when they scream for help. maybe we need to stop trying to chemically fix what we broke with our plates…
mike swinchoski
January 27, 2026 AT 12:21Genes? Please. I know a guy who took statins and got muscle pain. He ate more meat, stopped drinking soda, and now he’s fine. No test needed. Just stop being weak.
Trevor Whipple
January 28, 2026 AT 16:52everyone keeps saying "switch to rosuvastatin" like it's magic. i did. still got pain. then i tried ezetimibe. still pain. turns out i have a rare CACNA1S variant nobody tests for. so now i'm just taking niacin and praying. thanks for the false hope, science.
Gregory Parschauer
January 30, 2026 AT 00:45Let’s be brutally honest: this entire pharmacogenomic movement is a corporate marketing ploy dressed up as science. SLCO1B1 explains 6% of cases? Then why are labs pushing $400 tests? Why are hospitals billing insurers for it? Because they’re making money off your confusion. The real solution? Lower doses. Lifestyle changes. And maybe-just maybe-stop treating every ache as a genetic emergency. You’re not broken. You’re just a human being in a broken system.
James Castner
January 30, 2026 AT 10:05Thank you for that perspective. But I’d argue it’s not about profit-it’s about equity. If a test can prevent one person from quitting their statin and having a heart attack at 52, isn’t that worth it? Yes, lifestyle matters. But for many, it’s not enough. We don’t tell diabetics to just eat less sugar and stop taking insulin. We don’t tell asthma patients to just breathe better and stop using inhalers. Why do we do that with statins? Because we still think of heart disease as something you "should have avoided." It’s not. It’s biology. And biology deserves better than guesswork.