Heat Therapy Benefits for Bladder Muscle Spasms and Urinary Tract Relief
 Oct, 13 2025
Oct, 13 2025
Heat Therapy Safety Checker
Check Your Heat Therapy Settings
Ensure your heat therapy application is safe and effective for bladder muscle spasms.
Important Safety Tips
For optimal and safe heat therapy:
- Never exceed 43°C (109°F)
- Limit sessions to 15-20 minutes
- Always use a barrier like a towel between heat source and skin
- Stay hydrated during therapy
Heat therapy is the practice of applying controlled warmth to body tissues to ease discomfort, improve blood flow, and relax tight muscles. For anyone dealing with painful bladder spasms or irritation of the urinary tract, a gentle heat source can be a game‑changer.
Key Takeaways
- Warmth relaxes the bladder’s detrusor muscle, reducing involuntary contractions.
- Improved circulation speeds up removal of inflammatory by‑products.
- Simple tools-heating pad, warm compress, or a soothing bath-are enough for most people.
- Heat works best for chronic spasms, not for acute infection‑related pain.
- Safety tips (temperature limits, time‑frames, skin checks) prevent burns.
How Heat Therapy Relaxes Muscle Spasms
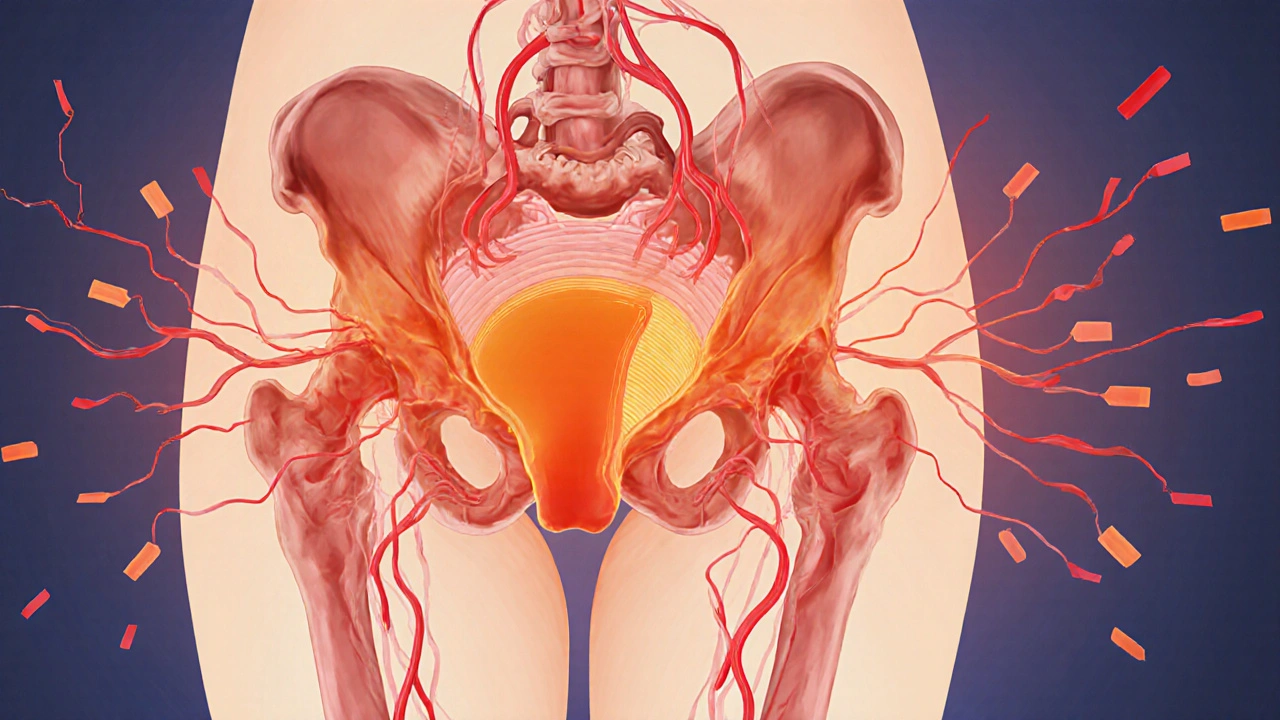
When the muscle spasm an involuntary, sustained contraction of a muscle fiber hits the bladder wall, the person feels a sudden urge to urinate or experiences sharp pelvic pain. The bladder’s detrusor muscle, a smooth muscle layer, is especially sensitive because it works around the clock, filling and emptying dozens of times a day.
Applying heat raises the temperature of the muscle fibers and surrounding connective tissue. This does three things:
- Increases blood flow, delivering oxygen and nutrients that help the muscle reset.
- Reduces the firing rate of nerve endings that send spasm signals.
- Softens the collagen in the pelvic floor, allowing the detrusor to stretch more comfortably.
Because the bladder a hollow muscular organ that stores urine before excretion and the urinary tract the network of kidneys, ureters, bladder, and urethra that moves urine out of the body share the same nerve supply, calming one area often eases the other.
Practical Ways to Apply Heat
Heat therapy can be delivered in several low‑cost, home‑friendly ways. Choose the method that fits your lifestyle and the area you need to target.
- Heating pad an electric or microwavable pad that provides steady warmth: Place it on the lower abdomen for 15‑20 minutes. Keep the temperature around 40‑43°C (104‑109°F) to avoid skin damage.
- Warm compress a cloth soaked in hot water and wrung out: Ideal for travel or work breaks. Swap it out every 5 minutes to maintain consistent heat.
- Hydrotherapy the use of warm water baths to soothe muscles and joints: A 20‑minute sit‑in a tub filled with water at about 38°C (100°F) relaxes the pelvic floor and detrusor simultaneously.
Whichever method you pick, remember to test the surface with the back of your hand before applying it to the skin.
Heat vs. Cold: A Quick Comparison
| Aspect | Heat Therapy | Cold Therapy |
|---|---|---|
| Primary effect | Muscle relaxation, increased circulation | Vasoconstriction, numbing of pain |
| Best for | Chronic spasms, tension‑type pelvic pain | Acute inflammation, swelling after injury |
| Typical duration | 15‑20minutes, 2‑3 times a day | 10‑15minutes, once after activity |
| Contraindications | Open wounds, severe skin conditions | Raynaud’s disease, cold‑sensitive nerves |
For bladder muscle spasms, heat consistently outperforms cold because the problem is stiffness, not swelling.
When Heat Therapy Shines-and When It Doesn’t
Heat works wonders for several urinary‑related conditions, but it isn’t a universal fix.
- Cystitis inflammation of the bladder wall, often caused by infection: Heat can soothe pain, but if an infection is present you still need antibiotics. Use heat only after the infection is cleared.
- Prostatitis inflammation of the prostate gland, sometimes causing urinary urgency: Gentle heat on the lower abdomen may reduce muscle tension that aggravates prostatitis symptoms.
- Kidney stones: Heat does not dissolve stones, but a warm bath can ease the surrounding muscle cramp that often follows stone movement.
- Pregnancy: The pelvic floor is already under extra strain. A low‑heat compress can be safe, but always check with a healthcare provider first.
If you have a fever, an active urinary infection, or skin conditions like eczema over the treatment area, skip heat until the underlying issue resolves.

Safety Tips to Get the Most Out of Heat
- Never exceed 43°C (109°F). Use a thermometer if your device doesn’t have a built‑in setting.
- Limit each session to 20 minutes. Overheating can cause muscle fatigue rather than relaxation.
- Place a thin towel between the heat source and skin to prevent burns.
- Stay hydrated. Warm tissues need fluid to support increased blood flow.
- Track your symptoms. Note any reduction in urgency, pain level, or frequency after each session.
Following these simple rules keeps heat therapy effective and risk‑free.
Frequently Asked Questions
Can I use a hot water bottle instead of a heating pad?
Yes, a hot water bottle works fine as long as you wrap it in a cloth and keep the temperature below 43°C. Check it every few minutes to avoid overheating.
How often should I apply heat for chronic bladder spasms?
Most people find relief with two to three 15‑minute sessions daily. Adjust based on how your symptoms respond.
Is it safe to combine heat therapy with medication for overactive bladder?
Generally, yes. Heat doesn’t interact with oral meds, but if you’re using topical anticholinergics, watch for skin irritation. Always check with your doctor.
What if I feel a burning sensation during treatment?
Stop immediately, remove the heat source, and cool the area with a damp cloth. The sensation may signal that the temperature is too high or the skin is too sensitive.
Can heat therapy help after pelvic floor physical therapy?
Absolutely. Warmth can enhance the benefits of stretching and strengthening exercises by keeping the muscles pliable between sessions.
Next Steps
If you’ve never tried heat therapy for bladder issues, start with a simple warm compress tonight. Record how often you feel the urge to go and whether the pain eases. Within a week you’ll know if the approach is helping. Should symptoms persist or worsen, schedule a check‑up-especially to rule out infection.

Jeremy Olson
October 13, 2025 AT 15:46I’ve found that a consistent 15‑minute warm compress applied to the lower abdomen can noticeably calm the detrusor muscle. Keeping the temperature under 43 °C and using a thin towel helps avoid skin irritation while still delivering therapeutic heat. Hydration is essential because warm tissues require adequate fluid to support increased circulation.
Ada Lusardi
October 16, 2025 AT 13:54Heat feels sooo soothing 😌🔥
Pam Mickelson
October 19, 2025 AT 12:02From my experience, a microwavable heat pack is a handy option for work breaks. Just test the surface with the back of your hand before you place it on your skin. I recommend a 5‑minute interval change to keep the temperature steady and safe.
Joe V
October 22, 2025 AT 10:10Sure, heat is great-if you enjoy feeling like a toasted marshmallow. Just don’t push it past 43 °C, unless you fancy a third‑degree burn. Remember, the goal is relaxation, not a sauna session.
Virat Mishra
October 25, 2025 AT 08:18People always ignore the moral side of self‑care and think it’s just a luxury. Using heat responsibly shows you respect your body, not just your convenience.
Mariah Dietzler
October 28, 2025 AT 05:27i think heat therapy is ok but dont overdo it srsly. a little warm pad is enough hey.
Hariom Godhani
October 31, 2025 AT 03:35When one delves into the nuanced art of thermal alleviation for bladder spasms, the layers of physiological interaction begin to unwind like a tapestry of gentle fire. The detrusor muscle, perpetually engaged in the rhythm of filling and emptying, becomes a prime candidate for the soothing influence of controlled heat. As temperature rises modestly within the safe corridor of 40‑43 °C, vasodilation escalates, ushering a surge of oxygen‑rich blood to the muscular fibers. This influx delivers the essential nutrients required for cellular repair while simultaneously flushing away metabolic waste that may perpetuate hyperexcitability. Moreover, the thermal stimulus dampens the firing rate of nociceptive afferents, thereby diminishing the perceived urgency that often haunts sufferers. The collagen embedded within the pelvic floor’s connective tissue undergoes a subtle softening, granting the detrusor greater elasticity and reducing the rigidity that fuels spasmodic contractions. In tandem, the sympathetic and parasympathetic pathways, which share a common innervation with the urinary tract, experience a recalibration that favors relaxation over spasm. Consistency, however, remains the keystone; two to three sessions daily, each meticulously timed to fifteen minutes, forge a habit that conditions the nervous system to accept a lower baseline of tension. It is paramount, nevertheless, to heed the advisory against exceeding the 43 °C threshold, for the line between therapeutic warmth and harmful burn is razor‑thin. Hydration, the unsung hero of this regimen, serves to amplify circulatory benefits while preventing the desiccation of tissues that could otherwise diminish heat conductivity. Should any sensation of burning emerge, immediate cessation and cooling are non‑negotiable, as they signal the breach of safe parameters. Ultimately, when harnessed with discipline and awareness, heat therapy transcends a mere comfort measure, evolving into a potent adjunct in the management of chronic bladder muscle spasms.
Joery van Druten
November 3, 2025 AT 01:43For those seeking a low‑cost solution, a simple hot water bottle wrapped in a towel works just as well as an electric pad. Make sure to rotate the bottle every few minutes to maintain even heat distribution. This method also avoids the temptation to set the device at a higher temperature than intended.
Melissa Luisman
November 5, 2025 AT 23:51Stop over‑complicating things-just follow the safety guidelines. Anything beyond that is unnecessary and potentially harmful.
Akhil Khanna
November 8, 2025 AT 21:59Hey folks 😊, remember to check your skin condition before any heat session-especially if you have eczema or a minor cut. A tiny burn can turn into a bigger problem, lol. Stay safe and keep those kidneys happy!
Zac James
November 11, 2025 AT 20:08From a cultural perspective, many traditional practices also rely on warmth for pelvic discomfort, reinforcing the scientific findings here.
Breanna Mitchell
November 14, 2025 AT 18:16I love how approachable this guide is-no jargon, just clear steps. It’s encouraging to see that something as simple as a warm compress can make a real difference. Keep sharing these practical tips!
Alice Witland
November 17, 2025 AT 16:24Oh great, another ‘miracle cure’ wrapped in HTML. If only a warm towel could solve everything, right? Let’s at least admit that it’s not a substitute for professional care.
Tammie Sinnott
November 20, 2025 AT 14:46While the post does a decent job outlining basic safety, it overlooks the nuanced role of thermoregulation in patients with autonomic dysfunction. Those individuals may experience exaggerated vasodilation, leading to hypotension even with modest heat exposure. Additionally, the interaction between heat therapy and anticholinergic medication warrants a brief discussion, as concurrent use can heighten skin sensitivity. Acknowledging these edge cases would elevate the guide from a generic overview to a truly comprehensive resource.