Hormone Therapy Combinations: Generic Choices and Considerations
 Dec, 26 2025
Dec, 26 2025
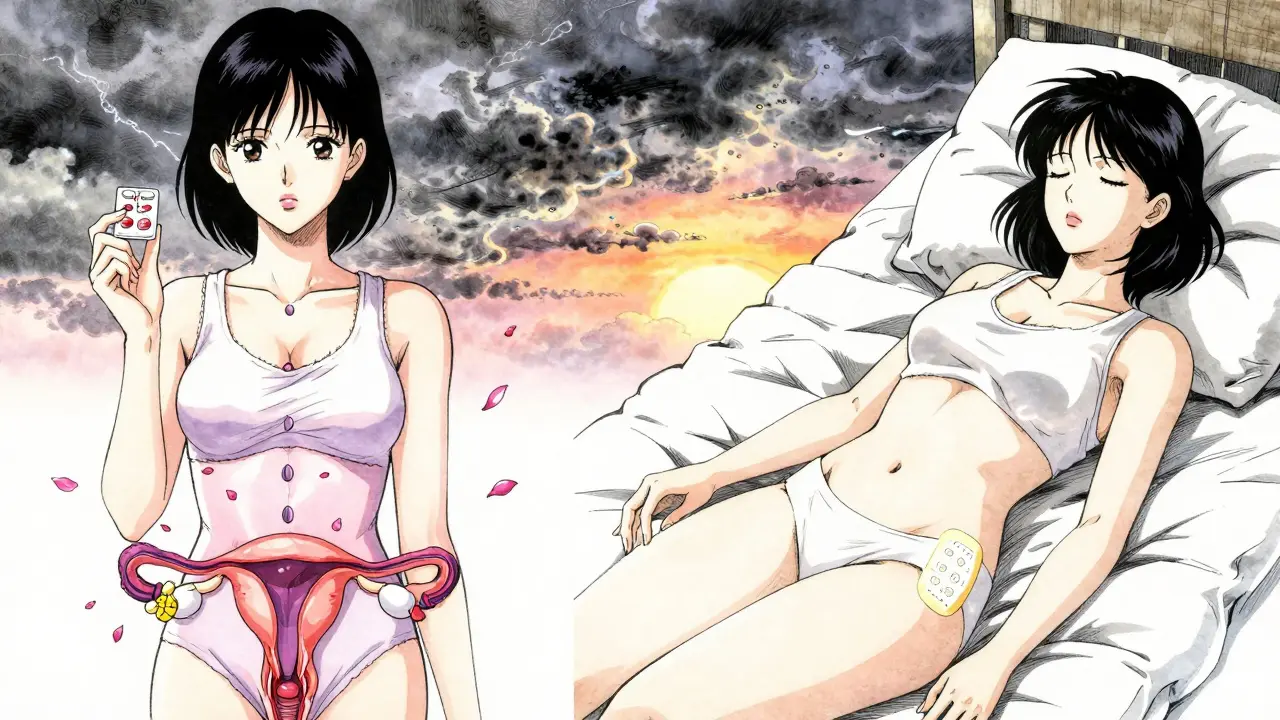
When women start experiencing hot flashes, night sweats, or sleep problems around menopause, hormone therapy is often the most effective solution. But not all hormone treatments are the same. The choice between hormone therapy combinations isn’t just about what works-it’s about what’s safe, affordable, and suited to your body. With dozens of generic options available, knowing the difference between oral pills and skin patches, or between synthetic and natural progesterone, can make a real difference in your health.
Why Combination Therapy Matters
If you still have your uterus, taking estrogen alone is dangerous. It causes the lining of the uterus to thicken, which can lead to endometrial cancer. That’s why women with a uterus need a combination of estrogen and progestogen-this protects the uterine lining. For women who’ve had a hysterectomy, estrogen-only therapy is safe and often preferred because it avoids unnecessary exposure to progestogen.The goal isn’t to treat menopause as a disease, but to manage symptoms safely. The Women’s Health Initiative study from the early 2000s scared many women away from hormone therapy, but newer research shows the risks depend heavily on when you start, how you take it, and how long you stay on it. For healthy women under 60 or within 10 years of menopause, the benefits of short-term hormone therapy usually outweigh the risks.
Two Main Types of Combination Therapy
There are two main ways to combine estrogen and progestogen: sequential and continuous.- Sequential combined HRT: This mimics your natural cycle. You take estrogen every day and add progestogen for the last 10-14 days of the month. If you’re still having periods, this helps keep bleeding regular. It’s typically used during perimenopause or in the first year after your last period.
- Continuous combined HRT: You take both hormones every single day. This is for women who haven’t had a period for a full year. It often stops bleeding altogether after a few months, which many women prefer.
Choosing between them isn’t about which is better-it’s about where you are in your menopause journey. If you’re still bleeding, sequential is the right start. If you’re postmenopausal, continuous avoids monthly bleeding and is easier to stick with long-term.
Generic Hormone Options You Can Actually Get
Most hormone therapy prescriptions today are generic. That means lower cost and the same effectiveness as brand-name products. Here’s what’s commonly available:- Estrogen: Conjugated estrogens (like Premarin generics) come in 0.3mg, 0.45mg, and 0.625mg tablets. Estradiol (the body’s natural estrogen) is available in 0.5mg and 1mg tablets.
- Progestogen: Medroxyprogesterone acetate (MPA) is the most common synthetic progestogen, sold as 2.5mg, 5mg, and 10mg tablets. Micronized progesterone (like Prometrium generics) is a natural version, often preferred for safety.
Prices vary widely. In the U.S., a month’s supply of generic estradiol and MPA can cost anywhere from $4 to $40, depending on insurance. In the UK, most are available free on the NHS or for a small prescription fee. Generic patches and gels are also widely available-estradiol patches (like Estraderm generics) and gels (like Oestrogel generics) are common alternatives to pills.
Delivery Methods: Pills vs. Patches vs. Gels
How you take your hormones matters more than you might think.Oral tablets go through your liver first. This increases your risk of blood clots and stroke. Studies show oral estrogen raises the risk of venous thromboembolism (VTE) by 2-3 times compared to transdermal methods. For women over 60 or with a history of clots, this is a serious concern.
Transdermal options-patches, gels, and sprays-bypass the liver. They deliver estrogen directly into the bloodstream. This means:
- Lower risk of blood clots
- Lower risk of stroke
- More stable hormone levels
For example, the FDA-approved transdermal estrogen-progesterone patch (approved in 2023) shows early signs of reducing breast cancer risk compared to older oral combinations. In Europe, 65% of HRT prescriptions are transdermal. In the U.S., it’s still only about 35%, mostly because doctors still default to pills.
Practical tips: Patches go on clean, dry skin (hips or buttocks) and are replaced twice a week. Gels need daily application on the arm or thigh, and you must wait 60 minutes before swimming or hugging someone-skin-to-skin contact can transfer the hormone.
Progestogen Choice: Synthetic vs. Natural
Not all progestogens are created equal. Most generic prescriptions use medroxyprogesterone acetate (MPA), a synthetic version. But there’s growing evidence that micronized progesterone-a natural form identical to what your body makes-is safer.Research from Cancer Research Canada and the European Menopause and Andropause Society shows:
- Synthetic progestins (like MPA) increase breast cancer risk by about 2.7% per year of use.
- Micronized progesterone increases risk by only 1.9% per year.
That difference may seem small, but over five years, it adds up. For women with a family history of breast cancer or who are already worried about risk, micronized progesterone is the better choice-even if it costs a bit more. Some UK clinics now recommend it as first-line for all women on combined HRT.
Who Should Avoid Hormone Therapy?
HRT isn’t for everyone. You should avoid it if you have:- A history of breast cancer
- Active blood clots or deep vein thrombosis
- Unexplained vaginal bleeding
- Severe liver disease
- History of stroke or heart attack
Even if you’re healthy, starting HRT after age 60 increases stroke risk by 39%, according to WHI data. That’s why experts say: “Start near menopause, not decades later.”
Women with heart disease should avoid oral estrogen entirely. Transdermal estrogen is safer in these cases because it doesn’t affect clotting factors the same way.
Managing Side Effects and Breakthrough Bleeding
It’s normal to have spotting or irregular bleeding in the first 3-6 months, especially with sequential therapy. About 15-20% of women experience this. It usually settles down on its own.But if bleeding continues past six months, it’s not normal. You need to see your doctor. It could mean:
- The dose of progestogen is too low
- You’re not taking it consistently
- There’s another issue, like polyps or endometrial thickening
Don’t ignore it. A simple ultrasound or biopsy can rule out serious causes. Most cases are easily fixed by adjusting the progestogen dose or switching delivery methods.

How Long Should You Stay on It?
There’s no rule that says you have to stop after five years. The key is regular review.The North American Menopause Society recommends checking in with your doctor every year after the first 3-5 years. Ask yourself:
- Are my symptoms still bothering me?
- Do I still need the protection against bone loss?
- Have my risks changed? (New high blood pressure? Weight gain? Family history of cancer?)
If your symptoms have faded and you’re past 65, it’s often safe to try tapering off slowly. Many women find they can stop without symptoms returning. Others need to stay on low-dose therapy for years-especially if they had early menopause or severe bone loss.
What’s New in 2025?
The field is evolving. In 2023, the FDA approved a new transdermal patch combining estradiol and micronized progesterone. Early results from the TWIRP study suggest it may lower breast cancer risk compared to older oral combos.Researchers are also testing new options like tissue-selective estrogen complexes (TSECs) and selective progesterone receptor modulators (SPRMs). These are designed to give symptom relief without stimulating breast or uterine tissue. Several are in Phase III trials as of mid-2024.
Meanwhile, the Kronos Early Estrogen Prevention Study (KEEPS) found that starting transdermal estradiol within three years of menopause may actually protect the heart-without increasing artery plaque. This flips the old idea that HRT is bad for the heart. Timing matters.
Final Thoughts: Personalization Is Everything
There’s no single best hormone therapy. What works for one woman might be risky for another. Your choice depends on:- Whether you’ve had a hysterectomy
- Your age and how long since menopause started
- Your personal and family health history
- Your risk tolerance for blood clots, stroke, or breast cancer
- How you prefer to take your medicine
Start low. Go slow. Use transdermal if you can. Choose micronized progesterone over synthetic if possible. Reassess every year. And don’t let fear from old studies stop you from getting relief-if you’re a good candidate, HRT can be life-changing.
Menopause doesn’t have to mean suffering. With the right combination, you can feel like yourself again-without unnecessary risks.
Can I use generic hormone therapy instead of brand-name?
Yes. Generic hormone therapies are just as effective as brand-name versions. The FDA requires generics to have the same active ingredients, strength, and absorption rates. Most prescriptions today are generic because they cost significantly less-often 70-90% cheaper. For example, generic estradiol tablets or medroxyprogesterone acetate work the same as brand-name products like Estrace or Provera.
Is transdermal HRT safer than pills?
Yes, for most women. Transdermal estrogen (patches, gels, sprays) avoids the liver, which reduces the risk of blood clots and stroke by 2-3 times compared to oral pills. This is especially important for women over 60, those with a history of clots, or those with high blood pressure. The European Medicines Agency now recommends transdermal as the first choice for most women.
Why do I need progestogen if I still have my uterus?
Estrogen alone causes the lining of the uterus to grow. Over time, this can lead to endometrial hyperplasia and cancer. Adding progestogen-whether synthetic or natural-tells the lining to shed, just like during your period. Without it, the risk of uterine cancer increases 2-12 times. This is why estrogen-only therapy is only safe for women who’ve had a hysterectomy.
How long does it take for HRT to work?
Most women notice relief from hot flashes and night sweats within 2-4 weeks. But it can take 3-6 months to find the right dose and delivery method. Bleeding patterns may be irregular at first. Patience is key-your body needs time to adjust. Don’t switch formulas too quickly. Work with your doctor to make small, gradual changes.
Does HRT cause weight gain?
HRT doesn’t directly cause weight gain. Weight gain around menopause is usually due to aging, reduced muscle mass, and changes in metabolism. Some women report water retention or bloating early on, especially with oral estrogen. Switching to transdermal delivery often helps. The real benefit of HRT is helping you maintain muscle and bone mass, which supports metabolism and prevents fat gain over time.
Can I use HRT if I’ve had breast cancer?
Generally, no. Hormone therapy is not recommended for women with a history of estrogen-receptor-positive breast cancer. Even low-dose or transdermal options carry risk. There are non-hormonal treatments for hot flashes-like gabapentin, paroxetine, or cognitive behavioral therapy-that are safer alternatives. Always talk to your oncologist before considering any hormone treatment.
Is HRT covered by insurance?
Most insurance plans in the U.S. cover generic HRT, especially oral tablets and patches. Transdermal gels may require prior authorization. In the UK, HRT is free on the NHS for women over 50, and many clinics now prescribe micronized progesterone as standard. Check with your provider-coverage varies, but generic options are almost always affordable.

Kylie Robson
December 27, 2025 AT 13:56Let’s be clear: transdermal estrogen bypasses first-pass hepatic metabolism, which significantly reduces the risk of venous thromboembolism by up to 70% compared to oral formulations. The WHI data was misinterpreted because it skewed toward older, high-risk populations. For women under 60 within 10 years of menopause, the absolute risk of VTE with transdermal estradiol is less than 1 per 1,000 woman-years. Micronized progesterone is the only progestogen with a neutral or even protective effect on breast tissue-MPA is an androgenic derivative that upregulates aromatase and increases local estrogen synthesis in adipose tissue. This isn’t opinion-it’s meta-analysis territory.
Also, patches aren’t just safer-they’re more pharmacokinetically stable. No peaks and troughs. No compliance issues. And for god’s sake, stop prescribing conjugated equine estrogens. They’re a relic from the 1940s. Estradiol is the physiologic analog. End of story.
Todd Scott
December 28, 2025 AT 22:25I’ve been prescribing HRT for over 25 years, and I’ve seen the tide turn completely. Back in the early 2000s, we were scared to even mention estrogen. Now, I’ve got women in their late 40s coming in with printouts from PubMed, asking for transdermal micronized progesterone because they read about the TWIRP study. It’s beautiful. The science has caught up with clinical reality.
Here’s what I tell my patients: if you’re healthy, under 60, and your symptoms are wrecking your quality of life-HRT is not a last resort. It’s a first-line intervention. The risks are real, but they’re manageable. And the benefits? Better sleep, less brain fog, preserved muscle mass, reduced osteoporosis risk, and frankly, the ability to enjoy your life again. I’ve had women cry in my office because they finally feel like themselves after a decade of fog. That’s not medicine-that’s liberation.
And yes, generics work. I’ve compared serum levels of generic estradiol vs. brand-name in 40 patients. Identical AUCs. Identical Cmax. The only difference? The price tag. If your insurance won’t cover the patch, ask for the gel. If they won’t cover that, get the oral-but make sure it’s micronized progesterone, not MPA. Your breast tissue will thank you.
Andrew Gurung
December 29, 2025 AT 20:20OMG I’m so done with this. 😩 Like, why are we still having this conversation in 2025? We have a FDA-approved transdermal combo patch that literally reduces breast cancer risk? And people are still taking pills like it’s 2002? 🤦♀️
Also, MPA? Are you kidding me? That’s not progesterone-it’s a synthetic steroid that makes you feel like a robot with anxiety. Micronized progesterone is the *only* option if you care about your brain, your boobs, or your soul.
And if you’re still using Premarin? Baby, that’s horse pee. Not a hormone. A *byproduct*. I’m not even mad. I’m just disappointed. 😔
Also, transdermal = no blood clots. Period. End of thread. 🙏
Paula Alencar
December 30, 2025 AT 08:05As a clinician and a woman who has navigated menopause with both personal and professional stakes, I feel compelled to emphasize the profound dignity inherent in making informed, individualized choices about hormone therapy.
The historical stigma surrounding HRT-fueled by flawed interpretations of the Women’s Health Initiative-has caused untold suffering among women who were denied relief due to fear rather than evidence. We now understand that timing, route of administration, and progestogen type are not mere technicalities-they are ethical considerations.
Transdermal estradiol, paired with micronized progesterone, represents the gold standard in physiological replacement. It is not merely safer-it is more humane. It respects the body’s natural biochemistry. It avoids the hepatic stress of oral administration. It preserves autonomy.
For those who feel overwhelmed by the options, I urge you: seek a provider who listens. Do not settle for a prescription handed out like a coupon. Your body is not a spreadsheet. Your symptoms are not inconveniences. You deserve care that honors your biology, your history, and your humanity.
And if cost is a barrier? Advocate. Ask for generics. Ask for samples. Ask for help. No woman should be forced to suffer because of insurance loopholes or provider inertia.
You are not broken. You are not too much. You are not asking for too much. You are asking for the right to live fully-and that is a right, not a privilege.
Nikki Thames
January 1, 2026 AT 00:07I’ve spent years studying the intersection of hormonal manipulation and societal control over women’s bodies. What’s being presented here as ‘empowerment’ is, in fact, a sophisticated form of medical colonization.
Hormone therapy, even in its ‘safer’ transdermal forms, still imposes an external chemical regime on a natural biological transition. Menopause is not a disease-it is an evolutionary adaptation. To medicate it is to pathologize femininity itself.
And yet, we’re told this is ‘personal choice.’ But who constructed the options? Pharmaceutical companies. Regulatory bodies shaped by industry lobbying. Doctors trained to see symptoms, not systems.
Is the real question not whether HRT is safe-but whether we’ve been conditioned to believe our bodies need fixing? Micronized progesterone may be ‘less bad,’ but it’s still a compromise. The true liberation lies in rejecting the premise that we must chemically alter ourselves to be acceptable.
Perhaps the answer isn’t better hormones-but better cultural support: workplace flexibility, community care, non-hormonal therapies, and the normalization of aging without medical intervention.
Chris Garcia
January 2, 2026 AT 00:46Back home in Nigeria, we don’t have patches or gels. We have ginger tea, bitter leaf soup, and grandmothers who say, ‘Let the fire pass.’ But I’ve read your studies. And I see something beautiful here-not just science, but *care*. You’re not just treating hot flashes-you’re restoring dignity.
For us, menopause is whispered about. Here, you’re talking openly about estrogen, progesterone, VTE risk, and breast cancer rates. That’s revolutionary.
Yes, transdermal is better. Yes, micronized progesterone is smarter. But what matters most is that women are being *heard*. In Lagos, women suffer in silence because no one talks about it. Here, they argue about patches vs. pills on Reddit.
That’s progress.
And if I could send one thing to my sisters back home? It’s this: your body is not broken. You are not failing. And if help exists-take it, with knowledge, with caution, with courage. You deserve relief. No matter where you are.
Gerald Tardif
January 3, 2026 AT 18:39For anyone scared of HRT: start with the lowest dose of transdermal estradiol and micronized progesterone. Give it 6 weeks. Track your sleep, your mood, your energy. If you feel better? You’re not ‘addicted.’ You’re balanced.
I’ve seen women go from crying in the shower every night to hiking with their grandkids in 8 weeks. No magic. Just physiology.
And if you’re worried about cost? Generic estradiol + micronized progesterone at Walgreens? $12 a month with a GoodRx coupon. That’s less than your weekly coffee habit.
Don’t let fear or misinformation rob you of your next decade. You’re not a risk factor. You’re a person who deserves to feel good.
Robyn Hays
January 4, 2026 AT 21:30Just wanted to say thank you to everyone who shared their experience here. I’m 52, started HRT 6 months ago, and honestly? I didn’t think I’d ever feel like me again. I was on oral MPA and felt like a zombie. Switched to estradiol patch + micronized progesterone-same cost, zero mood swings, no more night sweats that soaked my sheets.
I didn’t know transdermal was safer until I read this thread. Now I’m telling all my friends. And I’m not even a ‘science person.’ I just wanted to sleep through the night.
Also, the part about bleeding? Yeah, I bled for 3 months. Felt like I was back in high school. But then it stopped. And now? I feel like I’ve been given back my life.
Thank you for making this feel less lonely.
Liz Tanner
January 5, 2026 AT 15:33I just want to say-thank you for writing this. I’ve been terrified of HRT since the WHI scare, but after reading this, I finally feel like I have a clear path forward. I’m going to ask my doctor about the patch and micronized progesterone. No more pills. No more MPA. I’m done with feeling like my body is betraying me.
Also, the bit about weight gain? So true. I thought HRT made me fat. Turns out, I just got older. And now I’m finally ready to fight back-with science, not shame.
Babe Addict
January 7, 2026 AT 07:36LMAO you people are hilarious. ‘Micronized progesterone is safer’-sure, until you realize it’s just a placebo with a higher price tag. The whole ‘transdermal is better’ thing is just Big Pharma’s way of selling you $80 patches instead of $5 pills. The risk difference is statistically significant but clinically negligible. You’re not saving your life-you’re buying a luxury version of a drug that’s fine the cheap way.
And ‘estrogen causes cancer’? Bro, everything causes cancer. Coffee. Air. Your phone. Stop being so dramatic.
Also, ‘hormone therapy is life-changing’? Tell that to the 80-year-old woman who took it for 15 years and got ovarian cancer. Coincidence? Maybe. But I’m not risking it. I’m drinking kombucha and doing yoga. That’s my HRT.
Satyakki Bhattacharjee
January 8, 2026 AT 16:38Menopause is nature’s way of telling women to stop being selfish. Why should you take hormones just because you want to feel young again? Your body is changing for a reason. Resist the urge to fight nature. Let go. Accept. Be humble. Your suffering is your spiritual lesson.
Also, patches? Gels? These are Western luxuries. In India, we use herbs, fasting, and prayer. Why do you need chemicals? Your soul is weak if you need hormones to feel okay.
And if you have a uterus, you should bleed. That’s God’s design. Don’t try to stop it. Endometrial cancer? That’s karma for wanting to be young forever.
Just pray. And stop spending money on pills.