How Clomipramine Helps Treat Panic Disorder: What You Need to Know
 Nov, 18 2025
Nov, 18 2025
Clomipramine isn’t the first drug most people think of when they hear "panic disorder." SSRIs like sertraline or escitalopram get the spotlight. But for many who’ve tried those and still struggle with sudden, overwhelming fear - chest tightness, dizziness, the feeling that they’re dying - clomipramine can be the turning point. It’s not new. It’s not flashy. But in clinical practice, it’s one of the most effective medications for panic disorder, especially when other treatments fail.
What Clomipramine Actually Does
Clomipramine is a tricyclic antidepressant, or TCA. It was first developed in the 1960s and originally used for depression. But researchers noticed something unusual: patients with obsessive-compulsive disorder (OCD) improved more than those with depression alone. That led to deeper studies - and eventually, FDA approval for OCD in 1989. But its effect on panic attacks? That came from real-world use.
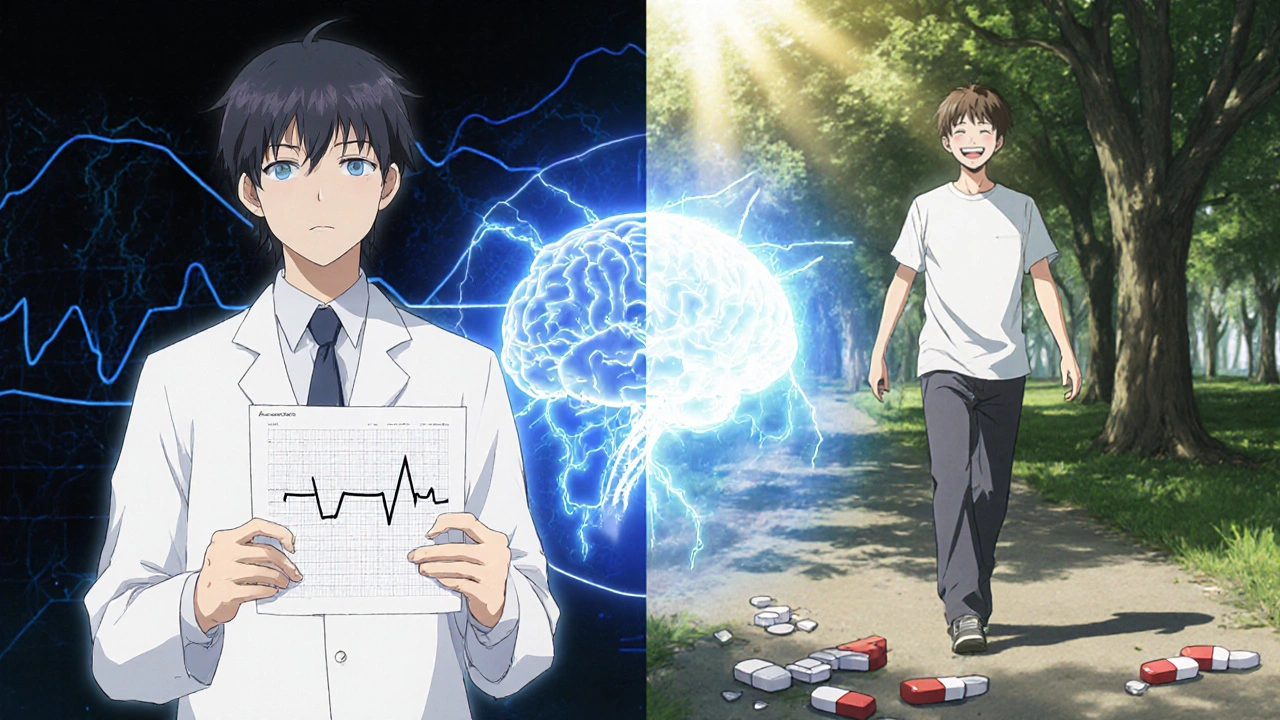
Unlike SSRIs, which mainly boost serotonin, clomipramine hits two neurotransmitters at once: serotonin and norepinephrine. This dual action seems to calm the brain’s fear circuitry more thoroughly. The amygdala - your brain’s alarm system - becomes less reactive. The hypothalamic-pituitary-adrenal axis, which triggers the stress response, doesn’t overfire as easily. In simpler terms: your body stops mistaking a normal heartbeat for a heart attack.
Studies show clomipramine reduces panic attacks by 60-70% in patients who complete a full course. One 12-week trial published in the Archives of General Psychiatry found that 68% of participants on clomipramine had at least a 50% drop in panic frequency, compared to 39% on placebo. That’s not just statistically significant - it’s life-changing.
Why It Works When Other Medications Don’t
Many people try SSRIs first. They’re safer. Fewer side effects. Easier to tolerate. But for about 30-40% of people with panic disorder, SSRIs just don’t cut it. Their panic attacks remain frequent, unpredictable, and debilitating. That’s where clomipramine steps in.
Why? Because panic disorder isn’t just about serotonin. Norepinephrine plays a huge role in the physical symptoms: rapid heartbeat, sweating, trembling, shortness of breath. Clomipramine blocks the reuptake of both chemicals, giving the brain a more balanced signal. SSRIs only touch serotonin. That’s why some people feel better mentally but still feel their body betraying them.
A 2021 meta-analysis in Journal of Clinical Psychiatry reviewed 17 randomized trials. It concluded that clomipramine was significantly more effective than SSRIs for reducing panic attack severity and preventing recurrence. The difference wasn’t huge for everyone - but for those with severe, treatment-resistant panic, it was the difference between staying home and going back to work.
The Side Effects: Real Talk
Clomipramine isn’t gentle. It’s not meant for casual use. Side effects are common, especially in the first few weeks.
- Dry mouth - almost universal
- Constipation - often worse than with SSRIs
- Drowsiness - makes it hard to drive or operate machinery early on
- Weight gain - average 2-5 kg over 6 months
- Blurred vision, dizziness, low blood pressure when standing
- Sexual dysfunction - decreased libido, delayed orgasm
Some people quit because of these. Others stick with it because the panic is worse. The key is starting low - usually 25 mg a day - and increasing slowly, often over 4-6 weeks. Most people reach 75-150 mg daily. Doses above 250 mg are rarely needed and increase risk.
There’s also a small but serious risk: clomipramine can affect heart rhythm. That’s why doctors check an ECG before starting, especially if you’re over 40 or have a history of heart issues. It’s not a drug you take without medical supervision.
How Long Does It Take to Work?
Don’t expect miracles in a week. Clomipramine doesn’t work like a benzodiazepine. You won’t feel calmer after one pill. It takes time - usually 4 to 8 weeks - for the brain to adapt. Some people notice small changes by week 3: fewer nighttime panic attacks, less dread before leaving the house. But full benefit? That’s often around week 10-12.
That’s why people give up too soon. They think it’s not working. They stop. Then they relapse. And they blame themselves. It’s not your fault. It’s just how this medicine works.
Doctors often recommend staying on clomipramine for at least 6-12 months after symptoms improve. Stopping too early increases relapse risk by 50%. Think of it like physical therapy for your brain. You need to keep practicing even after the pain fades.
Who Should Avoid It?
Clomipramine isn’t for everyone. It’s generally avoided in:
- People with recent heart attack or unstable heart disease
- Those with glaucoma (it can raise eye pressure)
- People with urinary retention or enlarged prostate
- Anyone taking MAO inhibitors (must wait at least 14 days after stopping an MAOI)
- Children under 18 - not approved for this age group
- Pregnant or breastfeeding women - data is limited, risks aren’t fully known
If you’re on other medications - especially sedatives, antihistamines, or certain painkillers - your doctor needs to check for interactions. Clomipramine can amplify drowsiness or lower blood pressure dangerously.

It’s Not a Standalone Fix
Clomipramine helps. But it doesn’t cure panic disorder by itself. The most successful outcomes come from combining it with therapy - especially cognitive behavioral therapy (CBT).
CBT teaches you how to recognize panic triggers, challenge catastrophic thoughts ("I’m having a heart attack"), and breathe through the physical sensations. Medication reduces the intensity. Therapy teaches you how to respond. Together, they break the cycle.
One study followed 120 people with severe panic disorder. Half got clomipramine alone. Half got clomipramine plus weekly CBT. After 6 months, 82% of the combo group were panic-free. Only 51% of the medication-only group were. Two years later, the combo group had a 30% lower relapse rate.
What Comes After Clomipramine?
Some people stay on clomipramine for years. Others taper off after 1-2 years and stay well. A few switch to SSRIs or SNRIs once their panic is under control.
But if you’ve tried multiple SSRIs and they didn’t work, don’t assume you’ve run out of options. Clomipramine is still the most potent option in the antidepressant class for panic disorder. It’s not the first line - but it’s the most reliable second line.
There are newer drugs like vilazodone or vortioxetine, but none have shown stronger results for panic than clomipramine. Ketamine and psychedelics are being studied, but they’re still experimental. For now, clomipramine remains the gold standard for treatment-resistant cases.
Final Thoughts: Is It Worth It?
If you’ve spent months avoiding places, skipping work, or lying awake terrified of the next attack - then yes. Clomipramine is worth the side effects. It’s worth the slow start. It’s worth the doctor visits and blood tests.
It’s not a magic pill. But for thousands of people, it’s the pill that brought them back to life. Not because it erased anxiety - but because it gave them the space to learn how to live with it.
If you’re considering it, talk to your doctor. Ask for the studies. Ask about your heart health. Ask about therapy. Don’t let fear of side effects stop you - but don’t rush into it either. This isn’t a quick fix. It’s a serious tool. And when used right, it can change everything.
Is clomipramine better than SSRIs for panic disorder?
For people who don’t respond to SSRIs, clomipramine is often more effective. Studies show it reduces panic attacks more significantly, especially when both serotonin and norepinephrine pathways are involved. However, SSRIs are usually tried first because they have fewer side effects. Clomipramine is typically reserved for treatment-resistant cases.
How long does it take for clomipramine to work for panic attacks?
Most people start noticing improvements in 4 to 6 weeks, but full benefits often take 8 to 12 weeks. It’s not an instant fix. Patience is key - stopping too early can lead to relapse. Doctors usually recommend staying on it for at least 6 months after symptoms improve.
Can clomipramine cause weight gain?
Yes, weight gain is common. On average, people gain 2 to 5 kilograms over 6 months. This is due to increased appetite and slower metabolism. It’s not inevitable - some people maintain their weight with diet and exercise - but it’s one of the most frequent reasons people discontinue the medication.
Is clomipramine addictive?
No, clomipramine is not addictive. It doesn’t produce euphoria or cravings. However, stopping it suddenly can cause withdrawal symptoms like dizziness, nausea, irritability, or flu-like feelings. That’s why doctors always recommend tapering off slowly over several weeks.
Can I drink alcohol while taking clomipramine?
It’s not recommended. Alcohol can increase drowsiness, dizziness, and low blood pressure - all side effects of clomipramine. Mixing them can also raise the risk of falls or accidents. Even moderate drinking can interfere with your recovery.
What happens if I miss a dose of clomipramine?
If you miss a dose, take it as soon as you remember - unless it’s close to your next scheduled dose. Don’t double up. Missing doses occasionally won’t cause panic to return immediately, but inconsistent use can make the medication less effective over time. Stick to your schedule as closely as possible.

Bette Rivas
November 19, 2025 AT 06:51Clomipramine’s dual reuptake inhibition is clinically significant because it targets both serotonin and norepinephrine pathways, which are hyperactive in panic disorder. SSRIs only modulate serotonin, leaving the noradrenergic system-responsible for physical symptoms like tachycardia and hyperventilation-largely untouched. That’s why patients often report feeling "mentally calmer" but still trapped in their bodies. The 68% response rate in the Archives study isn’t just a number; it’s people regaining their lives. The side effect profile is brutal, yes, but when panic is debilitating, tolerability becomes secondary to efficacy. Starting at 25mg and titrating slowly over 6 weeks isn’t just protocol-it’s survival strategy.
prasad gali
November 20, 2025 AT 13:35Let’s cut through the fluff. Clomipramine is a 1960s TCA with a half-life longer than your ex’s resentment. Yes, it works-when SSRIs fail, it’s the nuclear option. But you’re talking about dry mouth, orthostatic hypotension, QT prolongation, and weight gain that sticks like glue. If you’re not under close cardiac monitoring, you’re gambling with your life. And don’t even get me started on the withdrawal. This isn’t "mental health care," it’s pharmacological warfare. Use it only if you’ve exhausted every other option-and even then, document everything.
Paige Basford
November 21, 2025 AT 23:38Okay but real talk-I was on clomipramine for 9 months and it was a rollercoaster. First two weeks? I could barely get out of bed. Dry mouth felt like chewing cotton balls. Then around week 5, something clicked. I didn’t stop having panic attacks, but they stopped feeling like they were going to kill me. I started going to the grocery store again. Took me 3 months to feel like myself. And yeah, I gained 4 kilos. But I also got my job back. My therapist said the combo of med + CBT was the real game-changer. If you’re scared of side effects? Start low. Talk to your doc. Don’t give up at week 2. It’s not magic, but it’s damn close.
Ankita Sinha
November 22, 2025 AT 19:46Wait, so clomipramine is basically the OG panic weapon? I thought SSRIs were the gold standard, but now I’m seeing this is the secret sauce for treatment-resistant cases. 🤯 I’ve been on sertraline for a year and still panic at the sound of my own heartbeat. Maybe it’s time to ask my psych about this. Anyone know if insurance covers it? Also, how bad is the weight gain really? I’m already struggling with body image. 😅
Kenneth Meyer
November 23, 2025 AT 09:46There’s a quiet dignity in clomipramine’s obscurity. It doesn’t scream for attention like SSRIs or buzz like benzodiazepines. It just sits there, ancient and unglamorous, doing the hard work of restoring neural equilibrium. We’ve built a culture that wants quick fixes-pills that work in days, apps that cure anxiety in 10 minutes. But panic disorder isn’t a glitch. It’s a systemic collapse of the fear response. Clomipramine doesn’t fix the system; it rebuilds it, slowly, painfully, one synaptic adjustment at a time. The side effects aren’t flaws-they’re the cost of rewiring a brain that learned to scream at silence.
Donald Sanchez
November 23, 2025 AT 15:06bro clomipramine is the grim reaper of antidepressants 😭 i took it for 3 weeks and felt like a zombie who got hit by a truck made of dry socks and regret. weight gain? more like weight tsunami. also i had to pee every 10 mins but couldn’t actually go? 🤯 and don’t even get me started on the brain zaps when i missed a dose. BUT. after 2 months? i drove to the mall alone for the first time in 4 years. so yeah. worth it. kinda. maybe. 🤷♂️💊 #clomipraminewarrior #notadvice
Abdula'aziz Muhammad Nasir
November 24, 2025 AT 06:42As a clinician with over 15 years in psychiatric practice across three continents, I can confirm that clomipramine remains one of the most underutilized yet profoundly effective agents for severe, treatment-refractory panic disorder. Its mechanism-dual monoamine reuptake inhibition-is uniquely suited to the neurobiology of panic, which involves both limbic hyperactivity and autonomic dysregulation. While side effects are nontrivial, they are predictable and manageable with proper titration and monitoring. The key is patient education: setting realistic expectations about timelines, emphasizing the necessity of concurrent psychotherapy, and ensuring cardiac screening. This is not a drug for the faint of heart-but for those who have lost their way, it can be a lifeline.
Tara Stelluti
November 25, 2025 AT 18:56they say it works but i swear i cried for 3 days straight after my first dose like i’d lost my dog or something. like… why am i sobbing over a cereal commercial? i didn’t even like that cereal. then i realized-oh. my brain is rewiring. and it’s not pretty. i’m still on it. 8 months in. i can now go to the movies without checking every exit. but i still hate the taste of water. and my jeans don’t zip. worth it? i guess. but god. it’s a lot.