How Environmental Factors Influence Melanoma Risk
 Oct, 22 2025
Oct, 22 2025
UV Exposure Risk Calculator
UV Exposure Risk Assessment
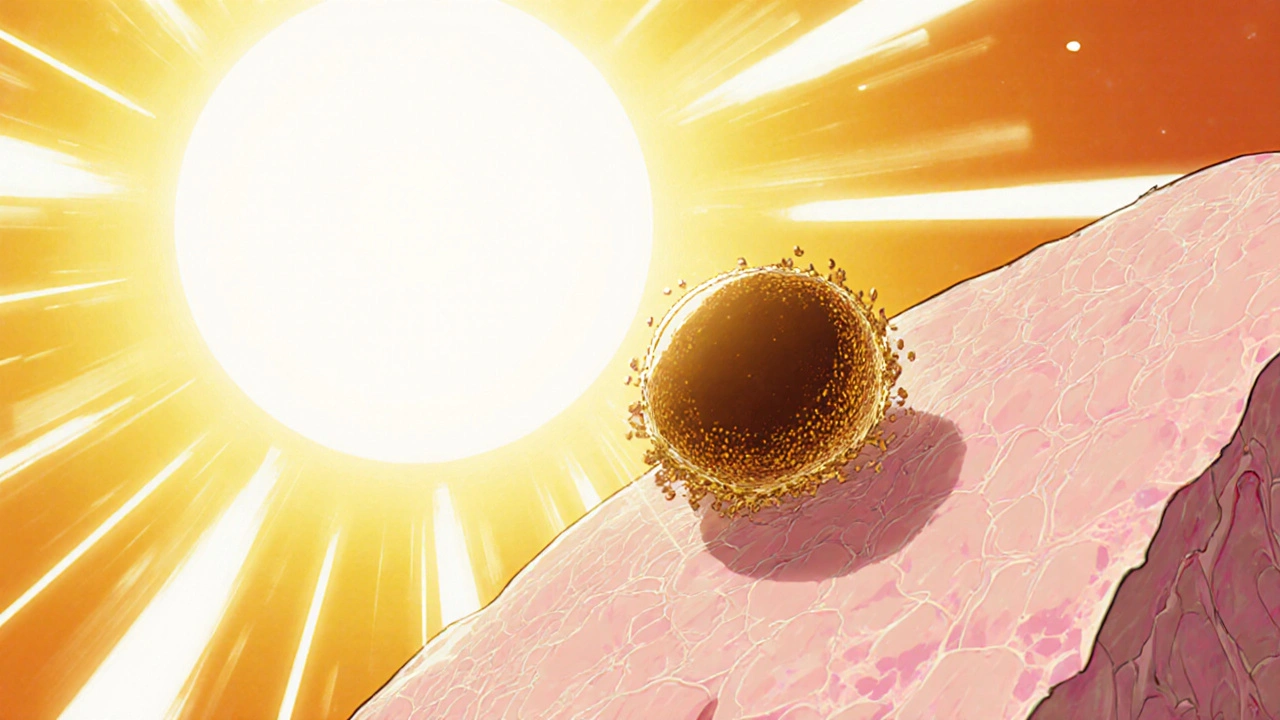
When you hear the word Melanoma is a type of skin cancer that originates in pigment‑producing cells called melanocytes. It’s the deadliest form of skin cancer, responsible for about 1% of all cancer deaths worldwide, yet it’s also one of the most preventable. The missing puzzle piece most people overlook is how the environment shapes that risk. By looking at sunshine, chemicals, and even climate change, you can see why melanoma isn’t just a genetic story.
Key Takeaways
- UV radiation from the sun and tanning beds is the single biggest environmental driver of melanoma.
- Geographic latitude, ozone depletion, and cloud cover create regional risk hotspots.
- Chemical agents such as pesticides, arsenic, and polycyclic aromatic hydrocarbons add a measurable risk.
- Climate change amplifies UV exposure and alters outdoor behavior, raising future melanoma incidence.
- Practical steps-sun protection, regular skin checks, and reducing chemical exposure-cut risk dramatically.
Understanding Melanoma
Melanoma develops when melanocytes mutate and begin to grow unchecked. The most common mutations involve the BRAF and NRAS genes, found in roughly 50% and 20% of cases respectively. While genetics set the stage, environmental triggers dictate whether those mutated cells become a dangerous tumor.
According to the World Health Organization, 324,000 new melanoma cases were diagnosed globally in 2022, up 30% from the 1990s. That surge mirrors rising UV exposure and industrial chemical use, not a sudden genetic shift.
What Counts as Environmental Factors?
In the context of skin cancer, "environmental factors" encompass anything outside the body that can influence melanocyte DNA. This includes natural elements like sunlight, man‑made sources such as tanning devices, and chemical agents that reach the skin either directly or via the bloodstream.
Below, we break down the biggest contributors and how they interact with personal risk.
UV Radiation - The Primary Culprit
Ultraviolet (UV) light splits into UVA (320‑400 nm) and UVB (280‑320 nm). UVB drives direct DNA damage, creating the classic cyclobutane pyrimidine dimers that mutate the BRAF gene. UVA penetrates deeper, generating reactive oxygen species that indirectly damage DNA.
Studies published in the Journal of Clinical Oncology (2023) estimate that >90% of melanoma cases have a history of significant UV exposure. Even intermittent, intense sunburns before age 35 double the lifetime risk.
Solar UV Index and Real‑World Exposure
The UV Index (UVI) quantifies how strong UV radiation is at a given place and time. A UVI of 6-7 is considered high; a value of 8+ signals very high risk. A single 30‑minute walk at a UVI of 9 can deliver the same DNA damage as a day at a UVI of 4 lasting two hours.
Tools like the EPA’s UV Index forecast let you plan outdoor activities around safer windows (UVI < 3) or ensure you wear protection.
Geographic Latitude, Altitude, and Ozone
Latitude matters: people living closer to the equator receive more UVB year‑round. A 2019 Australian study found melanoma rates 3‑4× higher in Queensland (22°S) than in Tasmania (42°S). Altitude also raises UV exposure; every 1,000 m up adds roughly 10% more UV intensity.
Ozone depletion thins the natural UV filter. The 2022 World Meteorological Organization report showed that the Antarctic ozone hole increased average UVB exposure by 5% over the past decade, with measurable skin‑cancer spikes in nearby Chilean coastal regions.
Artificial Sources: Tanning Beds
Tanning beds emit concentrated UVA, often at doses 10‑15 times stronger than midday sun. The International Agency for Research on Cancer classifies indoor tanning as a Group 1 carcinogen. A 2020 meta‑analysis linked a single tanning session before age 20 to a 75% higher melanoma risk later in life.
Occupational and Chemical Exposures
Beyond UV, certain workplace and environmental chemicals raise melanoma odds.
- Pesticides-especially organophosphates-have been linked to a 20% increase in melanoma among agricultural workers.
- Arsenic in drinking water creates skin lesions that can progress to melanoma; the US EPA limit of 10 ppb still leaves higher exposures in many regions.
- Polycyclic aromatic hydrocarbons (PAHs) released from diesel exhaust adhere to skin and generate DNA adducts.
Climate Change - A New Risk Amplifier
Warmer temperatures encourage longer outdoor periods and fewer cloud cover days, boosting cumulative UV dose. The Intergovernmental Panel on Climate Change (IPCC) projects a 0.5‑1 % annual increase in UV radiation for mid‑latitude regions by 2050.
Heatwaves also shift behavior: people trade indoor shielding for sun‑bathing, inadvertently raising their melanoma risk.
Air Pollution and UV Interaction
While particulate matter can scatter UV, certain pollutants like nitrogen dioxide actually increase UV‑induced skin damage by impairing DNA repair mechanisms. A 2021 European study found urban dwellers with high PM2.5 exposure had a 12% higher melanoma incidence than those in rural areas, even after adjusting for sun exposure.

Genetics Meets Environment
People with fair skin, freckles, or a family history of melanoma are genetically predisposed. However, research shows that environmental factors can override genetic protection. For example, a 2022 cohort of 2,000 individuals with MC1R variants showed that regular sunscreen use reduced their melanoma risk to the level of low‑risk genotypes.
Practical Prevention Checklist
- Check the daily UV Index; stay in shade or wear protective clothing when UVI ≥ 3.
- Apply broad‑spectrum SPF 30+ sunscreen 15 minutes before going outside; reapply every 2 hours.
- Avoid tanning beds entirely; seek alternative cosmetic options.
- Wear wide‑brim hats, UV‑blocking sunglasses, and UPF clothing during prolonged exposure.
- Inspect skin monthly; use the ABCDE rule for any new mole (Asymmetry, Border, Color, Diameter, Evolving).
- Limit exposure to known chemicals: wear gloves when handling pesticides, use water filters that reduce arsenic, and reduce time near diesel exhaust.
- Stay informed about local ozone alerts and climate‑related UV forecasts.
Following this checklist can shave years off your melanoma risk profile, even if you have a family history.
Future Outlook
As climate patterns shift and new chemicals enter the market, ongoing monitoring is crucial. Public health agencies are now pairing UV‑index apps with air‑quality alerts to give a fuller picture of skin‑cancer risk.
Research is also moving toward personalized risk scores that combine genetic data, skin type, and quantified environmental exposure. Expect a future where your smartwatch could warn you when today’s UV dose plus your personal risk crosses a danger threshold.
Quick Reference Table
| Factor | Typical Exposure | Relative Risk Increase | Mitigation |
|---|---|---|---|
| UVB Sunlight | 30 min midday, UVI 8+ | ≈ 2‑3× | Sunscreen, shade, clothing |
| UVA Tanning Bed | 10‑15 min session | ≈ 1.75× | Avoid indoor tanning |
| Pesticides (occupational) | Weekly handling | ≈ 1.2× | Protective gear, reduced use |
| Arsenic in water | Daily consumption >10 ppb | ≈ 1.3× | Filtration, source testing |
| High altitude (>1500 m) | Living/working at elevation | ≈ 1.1‑1.2× | Enhanced UV protection |
Frequently Asked Questions
Can a single sunburn cause melanoma?
A severe blistering sunburn, especially before age 35, significantly raises melanoma risk. While one burn alone isn’t a guarantee, it adds roughly a 20%-30% increase in lifetime odds.
Is sunscreen enough protection on a high‑UV day?
Sunscreen is essential but not sufficient. Combine it with shade, hats, and UV‑blocking clothing for full protection when UVI is 6 or higher.
Do people with darker skin need to worry about melanoma?
Yes, though the baseline risk is lower. UV exposure still damages DNA, and melanoma in darker skin often appears on less‑sun‑exposed areas, making regular skin checks crucial.
How does climate change affect my personal melanoma risk?
Warmer, clearer skies increase cumulative UV exposure. Over the next 30 years, average UV dose could rise by up to 10% in many regions, meaning you’ll need stricter sun‑protection habits.
Are there any dietary ways to lower melanoma risk?
A diet rich in antioxidants (vitamins C, E, and beta‑carotene) can help neutralize UV‑induced free radicals. While food alone won’t replace sun protection, it supports skin health.

Eileen Peck
October 22, 2025 AT 13:05Thans for the thorough breakdown, really eye‑opening.
Jonathan Harmeling
October 26, 2025 AT 18:33We need to hold ourselves accountable for the way modern life fuels melanoma risk, because ignorance is no excuse. The ubiquity of tanning salons screams profit over public health, and the glittering ads lure vulnerable teens into a deadly habit. UV‑rich vacations are marketed as status symbols, yet they ignore the long‑term cost on our skin. Pesticides sprayed across fields become invisible assassins that settle on our clothes and skin, and we turn a blind eye while corporate farms profit. Arsenic in drinking water is a silent killer that policymakers pretend doesn't exist, feeding a narrative that the environment is harmless. Climate change isn’t just about melting ice; it’s about longer, hotter days that tempt us to bask in harmful UV without protection. The ozone hole over the Southern Hemisphere is a reminder that our actions can thin the planet’s natural shield, yet we celebrate industrial growth like triumph. It is morally reprehensible that sunscreen, an essential public‑health tool, is often priced out of reach for low‑income families. We must demand universal access to affordable broad‑spectrum protection, not leave it to market forces. Education campaigns should be mandatory in schools, not optional flyer‑drops that get tossed into trash. The medical community should stop treating melanoma as an inevitable fate and start treating preventable exposure as a crime against future generations. Every sunburn before age 35 should be seen as a red flag, not a badge of bravery. The statistics on rising melanoma rates are not just numbers; they are stories of lives cut short by preventable harm. We owe it to our children to reshape cultural attitudes that glorify a suntanned look. In short, the environmental drivers of melanoma demand collective moral action, not passive acceptance.
Vandermolen Willis
October 31, 2025 AT 09:40Totally agree-protecting our skin should be a community effort 😊. The tips you listed are practical and easy to adopt, and they remind us that small daily habits add up to big safety gains. I love how you included both UV index monitoring and chemical exposure checks, because they’re often discussed separately. Let’s keep spreading this info so people actually use it, not just read it.
Steven Young
November 5, 2025 AT 00:46The sunscreen industry hides the truth about chemical filters they push onto us. They claim safety while long‑term studies are buried. Governments turn a blind eye because of lobbying money. Wake up and question what they put on your skin.
Kelly Brammer
November 9, 2025 AT 15:53Chemical exposure is a silent injustice that we can no longer ignore. Pesticides on crops, arsenic in drinking water, and PAHs from diesel exhaust infiltrate our bodies without consent. These agents amplify DNA damage and make skin cancer prevention far more complex than just sunscreen. We must demand stricter regulations and better public awareness, otherwise we are complicit in a hidden epidemic.
Ben Collins
November 14, 2025 AT 07:00Oh sure, because everyone has the time and money to become a full‑time toxicology lab, right? 🙄 While you’re busy sounding the alarm, most of us are just trying to get through the workday without a third cup of coffee. Maybe a simple reminder to wear gloves when handling chemicals would be more useful than a manifesto.
Marrisa Moccasin
November 18, 2025 AT 22:06Wow, you really think it's that simple, huh?, but what about the hidden agendas?, the big pharma and agro‑chemical lobbyists who've been feeding us misinformation for decades?, they profit from our ignorance, they fund research that downplays risks, and they market "clean" products that are anything but, we need to look behind the curtain, question every label, and demand transparency, otherwise we're just pawns in their profit game.
Caleb Clark
November 23, 2025 AT 13:13Listen up everyone, the climate crisis is not just about rising sea levels or melted glaciers. It’s also turning up the sun’s intensity and extending the hours we spend outdoors. That means more cumulative UV exposure for the average person, especially those who think a tan is a badge of honor. Hotter temperatures melt snow packs that used to reflect UV light, so we’re actually getting more direct sunlight hitting our skin. Erratic weather patterns push people into seeking shade under artificial structures where reflective surfaces can bounce UV rays back. The shift in agricultural zones forces workers into new environments with higher altitude and thinner ozone. All these factors combine to create a perfect storm for melanoma rates to skyrocket. We can’t treat this as a distant problem, it’s happening right now in our neighborhoods. Public health campaigns must link climate action to skin‑cancer prevention. Schools should teach kids about UV index alongside climate change lessons. Sunscreen manufacturers need to price products affordably, not just as a luxury. Governments should fund research on how climate‑driven UV changes affect different skin types. Communities can plant trees that provide natural shade in parks and streets. Individual choices like wearing UPF clothing become even more critical as UV doses rise. In short, fighting climate change is also fighting melanoma, and we can’t afford to ignore either.
Gary Marks
November 28, 2025 AT 04:20Yeah, right, as if anyone’s gonna read that novel‑length rant. Good luck convincing anyone.
Mary Keenan
December 2, 2025 AT 19:26Another overblown post, same old alarmist drivel.
Denver Bright
December 7, 2025 AT 10:33Wow, really?, you think shouting about climate and skin cancer actually changes anything?, maybe try a simpler approach next time?, because not everyone wants a lecture?, just a quick tip would do, don’t you think?
Kelli Benedik
December 12, 2025 AT 01:40😭 I’m literally shaking, this whole conversation feels like a rollercoaster of fear and hope! 🌞🌎 If we don’t act now, the future looks so dark, I can’t even… 😩