How to Avoid Liver Injury from OTC Pain Relievers
 Dec, 1 2025
Dec, 1 2025
Every year, thousands of people end up in the hospital not from a fall, a car crash, or a bad flu-but from something sitting right in their medicine cabinet. Acetaminophen, the active ingredient in Tylenol and hundreds of other over-the-counter pain relievers, is the leading cause of acute liver failure in the United States. It’s not because people are trying to harm themselves. Most of the time, they’re just trying to relieve a headache, back pain, or fever-and they don’t realize how easy it is to accidentally take too much.
Why Acetaminophen Is More Dangerous Than You Think
Acetaminophen is everywhere. It’s in Tylenol, but also in Excedrin, NyQuil, Vicodin, Percocet, and dozens of cold and flu remedies. More than 600 medications contain it. That’s the problem. People take one pill for a headache, then another for a fever, then a cold medicine that also has it-and suddenly they’ve hit 5,000 mg in a day. The safe limit? 4,000 mg for healthy adults. For someone with liver disease, it’s 2,000 mg. And if they’ve had even one drink? That threshold drops even lower.
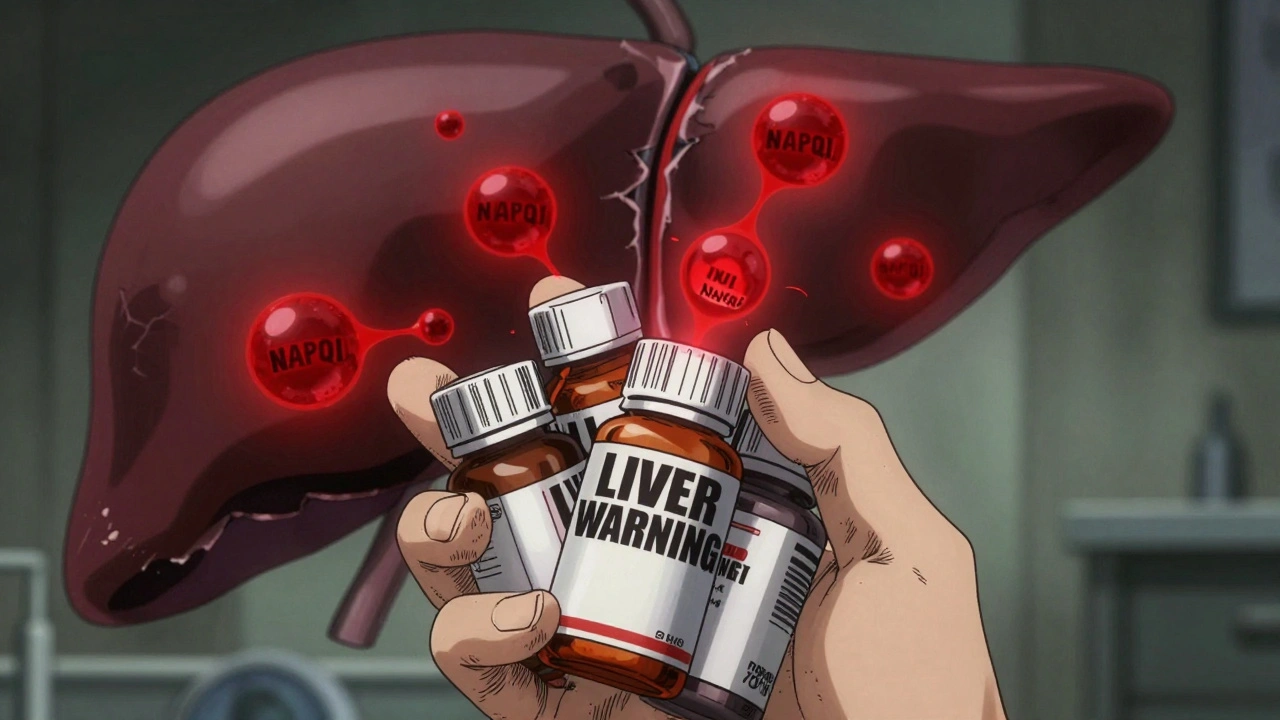
The body breaks down acetaminophen into harmless byproducts-but when you take too much, it creates a toxic chemical called NAPQI. Normally, your liver uses glutathione to neutralize it. But when you overload the system, glutathione runs out. That’s when NAPQI starts killing liver cells. It’s silent. You won’t feel anything until it’s too late.
The Hidden Dangers of Combination Medications
One of the biggest reasons people overdose on acetaminophen is because they don’t know it’s in their medicine. A 2022 FDA report found that about 25% of unintentional overdoses happen because people take multiple products that all contain acetaminophen. You take a cold tablet for your stuffy nose. Then you take a painkiller for your sore throat. Then you grab a sleep aid because you can’t rest. All three have acetaminophen. You think you’re being careful. You’re not.
Check every label. Look for the words “acetaminophen,” “APAP,” or “paracetamol.” If you see any of those, you’re taking it. Don’t assume because it’s a “natural” or “herbal” remedy that it’s safe. Some supplements contain hidden acetaminophen. Even some weight-loss products do.
What If You Have Liver Disease?
If you have hepatitis, fatty liver, cirrhosis, or any kind of chronic liver condition, your liver is already working hard. It doesn’t have extra capacity to handle extra toxins. The Veterans Affairs Hepatitis Resource Center and University Hospitals both say: if you have liver disease, never take more than 2,000 mg of acetaminophen in a day. That’s just four extra-strength pills. And absolutely no alcohol. Even one beer can make a 2,000 mg dose dangerous.
Some people think acetaminophen is safe for liver patients because it’s often recommended over NSAIDs. That’s true-but only if you stick to the lower dose. Pushing past 2,000 mg when your liver is damaged is like driving a car with a broken brake pedal. You think you’re in control. You’re not.
NSAIDs Aren’t the Safe Alternative
People often switch to ibuprofen or naproxen thinking they’re safer for the liver. They’re not. Diclofenac, in particular, is one of the most likely NSAIDs to cause liver injury. While NSAIDs don’t usually cause direct liver damage like acetaminophen, they can trigger kidney problems, stomach bleeding, and high blood pressure-especially in people with existing health conditions.
For someone with advanced liver disease, NSAIDs are even riskier. They can reduce blood flow to the kidneys, which are already under stress. That’s why the PMC 2023 review says NSAIDs are “particularly discouraged” in cirrhosis patients. The liver and kidneys work together. Damage one, and you strain the other.
What to Do Instead: Safer Pain Relief Options
If you need pain relief and you’re worried about your liver, here’s what actually works:
- Topical NSAIDs: Gels or patches with diclofenac or ibuprofen applied to the skin deliver pain relief without putting stress on your liver. They’re great for sore muscles or arthritis.
- Physical therapy: For chronic back or joint pain, movement and strengthening exercises reduce reliance on pills. Studies show they’re as effective as medication for many types of pain.
- Cognitive behavioral therapy (CBT): This isn’t just for anxiety. CBT helps people reframe how they experience pain, reducing the need for drugs.
- Acupuncture: Multiple studies, including those from the American Liver Foundation, show acupuncture helps with chronic pain without affecting liver enzymes.
- Heat and cold therapy: A warm bath or ice pack can ease inflammation and muscle pain without any chemicals.
The American Liver Foundation now recommends these non-drug options as first-line treatments for chronic pain-before you even reach for a pill.
How to Use Acetaminophen Safely
If you must use acetaminophen, follow these rules:
- Never exceed 4,000 mg per day (even if you feel fine).
- Stick to 1,000 mg per dose. Wait at least 8 hours between doses.
- If you have liver disease, cap it at 2,000 mg per day.
- Avoid alcohol completely while taking it-even one drink can double your risk.
- Use a pill organizer with daily limits marked. Write “NO ACETAMINOPHEN” on your cold medicine bottle if it has it.
- Keep a medication diary. Write down every pill you take, including brand names and doses.
And here’s a trick: when you buy a new medicine, hold it up to the light. Look at the front label. Since 2022, the FDA requires all OTC acetaminophen products to have a bold “LIVER WARNING” on the front. If it’s not there, it’s not compliant. Don’t buy it.
Recognizing the Warning Signs
Liver injury from acetaminophen doesn’t come with a siren. It creeps in. You might feel fine for hours, even a day. Then:
- You feel nauseous or start vomiting.
- You lose your appetite completely.
- You’re unusually tired-even after sleeping.
- You feel pain under your right ribs.
- Your urine turns dark, like tea.
- Your stool looks pale or clay-colored.
- Your skin or eyes turn yellow.
The National Institute of Diabetes and Digestive and Kidney Diseases says 93% of people with acetaminophen-induced liver failure show these symptoms within 24 to 72 hours. If you’ve taken acetaminophen and you notice even one of these, go to the ER. Don’t wait. Don’t call your doctor. Go.

The Antidote: Time Is Everything
If you or someone else has taken too much acetaminophen, there’s a treatment: N-acetylcysteine (NAC). It’s an antidote that can save your liver-but only if given fast. The American Association of Poison Control Centers says it’s most effective within 8 hours of overdose. After 16 hours, its power drops sharply. After 24 hours, it’s often too late.
That’s why knowing the signs matters. If you suspect an overdose-even if you’re not sure-call Poison Control (1-800-222-1222 in the U.S.) or go to the hospital immediately. Don’t wait for symptoms. Don’t hope it’ll pass. Liver damage from acetaminophen doesn’t reverse itself.
What’s Changing? The Future of Pain Relief
Researchers are working on new painkillers that don’t go through the liver at all. The NIH has invested $47 million since 2024 into developing analgesics with minimal liver metabolism. Some are already in early trials.
Meanwhile, genetic testing is becoming more common. Companies like 23andMe now offer tests that can tell you if you have a genetic variation that makes you more likely to build up toxic NAPQI. If you have this variant, your safe dose might be as low as 2,000 mg-even if you’re healthy.
Public awareness campaigns like the Acetaminophen Awareness Coalition’s “Know Your Dose” have cut pediatric overdoses by 35% since 2019. But adult overdoses? Still around 15,000 a year. That’s preventable.
Final Thought: Your Liver Can’t Tell You When It’s Overloaded
Your liver doesn’t scream. It whispers. By the time it shouts, it’s too late. You don’t need to avoid acetaminophen forever. But you do need to treat it like a powerful medicine-not a harmless candy. Read every label. Track every dose. Never mix it with alcohol. And if you have liver disease, ask your doctor before you take even one pill.
Pain is uncomfortable. But liver failure is life-changing. You don’t have to choose between the two. You just have to be smart.
Can I take acetaminophen if I have a fatty liver?
Yes-but only up to 2,000 mg per day, and never with alcohol. Fatty liver means your liver is already under stress. Even small overdoses can cause serious damage. Stick to the lower limit, and avoid any combination products that hide acetaminophen in cold or sleep meds.
Is ibuprofen safer for the liver than acetaminophen?
It depends. Ibuprofen doesn’t cause direct liver damage like acetaminophen, but it can harm your kidneys and stomach, especially if you have liver disease. For people with cirrhosis, NSAIDs like ibuprofen are often riskier than low-dose acetaminophen. Always talk to your doctor before switching.
How do I know if a medicine contains acetaminophen?
Look for “acetaminophen,” “APAP,” or “paracetamol” on the label. It’s in more than 600 products, including cold, flu, sleep, and migraine remedies. Since 2022, U.S. law requires OTC acetaminophen products to have a bold “LIVER WARNING” on the front. If you don’t see it, the product may not be compliant-avoid it.
What should I do if I think I took too much acetaminophen?
Call Poison Control at 1-800-222-1222 or go to the nearest emergency room immediately. Don’t wait for symptoms. The antidote, N-acetylcysteine (NAC), works best within 8 hours. After 16 hours, it’s much less effective. Time is the most important factor in saving your liver.
Can I drink alcohol while taking acetaminophen?
Never. Even one drink can lower your safe acetaminophen threshold to as little as 2,000 mg per day. Alcohol and acetaminophen together create a deadly mix that overwhelms your liver’s ability to detoxify. This combination is responsible for many hospitalizations each year. If you drink, don’t take it. If you take it, don’t drink.
Are there natural alternatives to OTC pain relievers?
Yes. Topical creams with menthol or capsaicin can ease muscle pain. Heat pads and ice packs help with inflammation. Physical therapy, acupuncture, and cognitive behavioral therapy are proven to reduce chronic pain without drugs. For many people, these options are safer and more sustainable than pills.
Should I get genetic testing for acetaminophen sensitivity?
If you’ve had unexplained liver enzyme spikes or take acetaminophen regularly, it might be worth considering. Some people have genetic variations that make them process acetaminophen slower, increasing their risk of toxicity-even at normal doses. Companies like 23andMe offer tests that can identify these variants. Talk to your doctor about whether it’s right for you.
Next Steps: Protect Your Liver Today
- Go through your medicine cabinet. Remove any expired or unnecessary pills.
- Write down every medication you take daily, including OTC and supplements.
- Check every label for acetaminophen. If you’re unsure, ask your pharmacist.
- Set a phone reminder: “No acetaminophen after 8 PM.”
- Consider switching to non-drug pain relief methods for chronic issues.
Your liver doesn’t ask for much. Just respect its limits. One pill at a time. No more. No less.

John Biesecker
December 2, 2025 AT 06:56Genesis Rubi
December 2, 2025 AT 19:10Doug Hawk
December 2, 2025 AT 22:01John Morrow
December 3, 2025 AT 19:13Kristen Yates
December 4, 2025 AT 14:38Saurabh Tiwari
December 6, 2025 AT 07:58Michael Campbell
December 7, 2025 AT 02:56Victoria Graci
December 8, 2025 AT 08:03Saravanan Sathyanandha
December 10, 2025 AT 04:31alaa ismail
December 11, 2025 AT 02:23ruiqing Jane
December 11, 2025 AT 22:44Fern Marder
December 13, 2025 AT 07:07Anthony Breakspear
December 13, 2025 AT 20:09