How to Prevent Wrong-Dose Errors with Liquid Medications: A Practical Guide for Patients and Providers
 Jan, 22 2026
Jan, 22 2026
Every year, thousands of children and adults receive the wrong amount of liquid medicine-not because someone made a careless mistake, but because the system is still built on outdated, confusing practices. A 2023 study in the Journal of Pediatrics found that 80% of pediatric home medication errors involve incorrect liquid doses. That’s not rare. That’s routine. And it’s preventable.
Why Liquid Medications Are So Risky
Liquid medications are tricky because they’re measured in tiny amounts. A child’s dose might be 2.5 mL. An adult’s might be 15 mL. But if you’re using a kitchen spoon, a dosing cup with blurry markings, or worse-guessing-you’re playing Russian roulette with safety.Here’s what goes wrong:
- Parents use teaspoons or tablespoons because they’re handy. But a household teaspoon holds anywhere from 3 to 7 mL-not the standard 5 mL.
- Pharmacies hand out dosing cups with both milliliters and teaspoons on the side. That confuses people. One study showed 41% of caregivers gave doses over 20% too high when using these cups.
- Look-alike bottles. Two different medications in similar packaging? Easy to grab the wrong one.
- Prescriptions still say “give 1 tsp.” Even though the American Academy of Pediatrics banned that in 2015, it still happens.
These aren’t just minor mistakes. They lead to hospitalizations, organ damage, and even death. The Institute for Safe Medication Practices lists wrong-dose liquid errors as one of the top 10 persistent medication hazards in 2024.
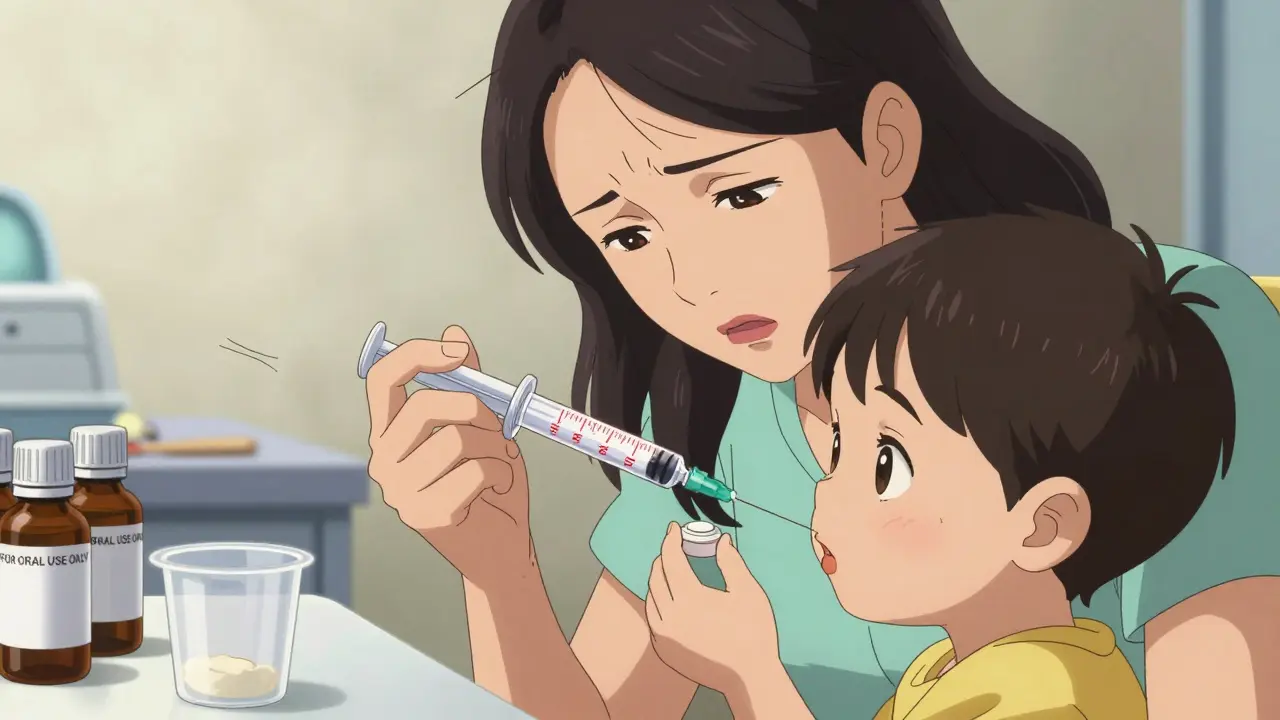
The #1 Fix: Ditch the Cup, Use the Syringe
The single most effective change? Stop using dosing cups for doses under 5 mL. Use an oral syringe instead.Here’s why:
- Oral syringes with 0.1 mL graduations are 37% more accurate than dosing cups, according to a Yale study published in Pediatrics.
- For a 2.5 mL dose, syringes are 94% accurate. Dosing cups? Only 76%. Household spoons? Just 62%.
- The American Academy of Family Physicians now recommends syringes-only distribution for all pediatric liquid meds since 2020.
Don’t assume the pharmacy will give you one. Ask for it. Demand it. If they say, “We don’t have them,” tell them you’ll go elsewhere. A 1 mL oral syringe costs less than a dollar. It’s not a luxury-it’s a safety tool.
Units Matter: Milliliters Only
If a prescription says “1 tsp” or “2 tbsp,” that’s a red flag. Those units are outdated, vague, and dangerous.Milliliters (mL) are the only unit that should be used. Why?
- One teaspoon is not always 5 mL. It can be 3 mL or 7 mL depending on the spoon.
- Dr. Michael Cohen of ISMP says teaspoon and tablespoon measurements cause 28% of preventable pediatric errors each year.
- The American Society of Health-System Pharmacists (ASHP) mandates that all liquid meds must be dispensed with mL-only labeling.
When you get a prescription, check the label. If it says “tsp,” ask the pharmacist to rewrite it in mL. If they refuse, report it. This isn’t bureaucracy-it’s survival.
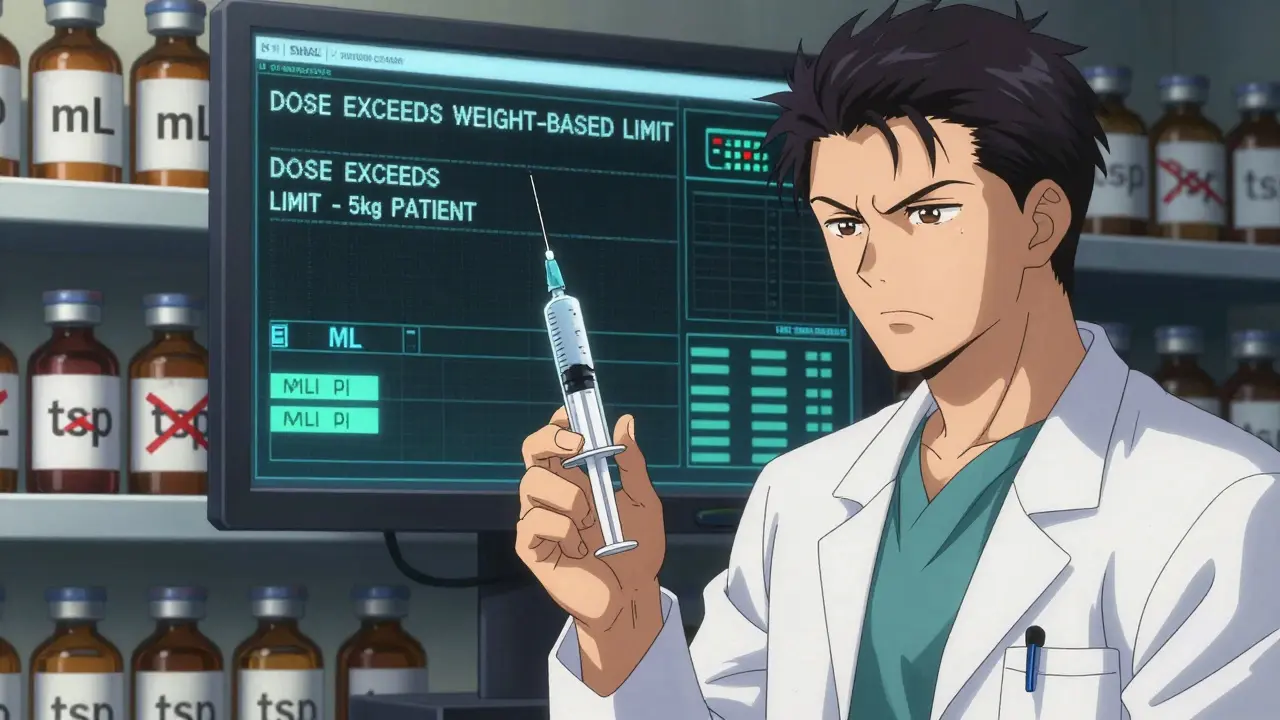
Technology Can Help-If It’s Used Right
In hospitals, technology is making a real difference:- Barcode Medication Administration (BCMA): Nurses scan the patient’s wristband and the medication. If the dose doesn’t match, the system alerts them. This cuts errors by 48%-but only if used 100% of the time.
- Electronic Health Records (EHR) with Clinical Decision Support: These systems check the dose against the patient’s weight. If you’re prescribing 10 mL for a 5 kg baby, the system flags it. One 2023 Cochrane Review showed this reduces errors by 58%.
- ENFit Connectors: Since 2016, all enteral (tube-fed) medication connectors must be incompatible with IV lines. This prevents deadly mix-ups. Hospitals using ENFit saw a 98% drop in wrong-route errors.
But here’s the catch: these tools only work if everyone uses them. A 2023 study in the Journal of Patient Safety found that BCMA systems failed to prevent errors in 32% of cases because staff bypassed them to save time.
What Pharmacies Should Be Doing
Pharmacies are on the front lines. They’re the last checkpoint before the medicine reaches you. Here’s what they need to do:- Always include an oral syringe with every pediatric liquid prescription.
- Print labels in bold, clear font with only mL and no teaspoons.
- Use amber-colored bottles with “FOR ORAL USE ONLY” labels-this reduces look-alike errors by 42%.
- Offer a 15-minute counseling session with every new liquid med. Show the caregiver how to use the syringe.
HealthyChildren.org surveyed 1,500 caregivers. 82% said they preferred syringes. But only 54% actually received one. That gap is unacceptable.
What You Can Do at Home
You don’t need a hospital budget to keep your family safe. Here’s your action plan:- Always ask for an oral syringe when picking up liquid medicine. If they don’t have one, say, “I need one to give this safely.”
- Throw away dosing cups. They’re not accurate enough.
- Never use kitchen spoons. Ever.
- Write down the dose in mL on a sticky note and keep it with the medicine.
- Double-check the label: Does it say mL? Is the number matching what the doctor said?
- Take a photo of the syringe at the correct level before giving the dose. It helps avoid second-guessing.
One mother on Reddit shared that she used a kitchen spoon for her son’s antibiotics-and gave him 3x the dose. He ended up in the ER. “I didn’t know teaspoons weren’t safe,” she wrote. “No one told me.”

Why This Isn’t Just a Parent Problem
This isn’t only about kids. Adults on liquid pain meds, anticoagulants, or seizure drugs are at risk too. A 2024 AllNurses.com survey found that 71% of medication errors nurses witnessed involved liquid formulations. The top causes? Similar-looking bottles and rushed administration.Older adults with vision problems, dementia, or shaky hands are especially vulnerable. A dosing cup with tiny lines? Nearly impossible to read. An oral syringe with clear markings? Life-saving.
The Bigger Picture: System Change Is Coming
Change is happening-but slowly.- The FDA’s 2024 draft guidance requires all over-the-counter liquid meds (like cough syrup) to come with an enclosed dosing device that meets ASTM F3100-23 standards. That means metric-only, no spoons.
- By 2026, all certified electronic health records must include pediatric dose-checking.
- ECRI Institute named liquid medication errors the #1 health technology hazard for 2024.
Some hospitals are ahead of the curve. Kaiser Permanente’s safety program reduced errors by 92% by mandating syringes, EHR alerts, and pharmacist-led education.
But rural clinics? They still struggle. 84% say cost is a barrier. 72% say staff don’t have time for training. That’s why your role as a patient or caregiver matters. You can demand better-even if the system hasn’t caught up yet.
Final Thought: Safety Is a Habit, Not a One-Time Fix
Preventing wrong-dose errors isn’t about buying fancy gadgets. It’s about changing habits:- Always use an oral syringe.
- Always read the label in mL.
- Always double-check.
- Always ask questions.
If you’re a parent, grandparent, or caregiver-you’re the last line of defense. Don’t assume someone else has it covered. If you’re a nurse, pharmacist, or doctor-don’t assume the patient knows how to use the syringe. Show them. Again. And again.
Because in medicine, a drop too much-or too little-can change everything.
Why can’t I just use a kitchen spoon to give liquid medicine?
Kitchen spoons vary in size-anywhere from 3 to 7 milliliters-while a proper teaspoon is exactly 5 mL. Using a spoon means you’re guessing the dose. For a child, that could mean giving 2x or 3x the right amount, leading to overdose, sedation, or even organ damage. Oral syringes are precise, affordable, and designed for this exact purpose.
What should I do if the pharmacy doesn’t give me a dosing syringe?
Ask for one. Say, “I need an oral syringe to give this safely.” If they say no, ask to speak to the pharmacist. If they still refuse, go to another pharmacy. A 1 mL syringe costs less than a dollar. It’s a standard safety tool, not a luxury. You have the right to receive it with every liquid prescription.
Is it safe to use a dosing cup if I’m careful?
For doses under 5 mL, no. Studies show dosing cups have error rates of 41% for small doses-compared to just 8% with oral syringes. Even careful users misread the lines, especially if the cup has both mL and tsp markings. For anything under 5 mL, use a syringe. For larger doses (like 10 mL or more), a syringe is still better, but a dosing cup can be acceptable if it has clear, bold mL markings and no other units.
What’s the difference between mL and tsp on a label?
mL (milliliters) is a precise metric unit. tsp (teaspoon) is a vague, household measure that varies by country and even by spoon. In the U.S., a teaspoon is supposed to be 5 mL, but most kitchen spoons aren’t. The American Academy of Pediatrics banned tsp from prescriptions in 2015 because it causes errors. Always insist on mL-only labeling.
Can I reuse an oral syringe for multiple doses?
No. Oral syringes should be used once per dose and then discarded. Reusing them can lead to contamination, especially if the tip touches surfaces, your child’s mouth, or other liquids. Some syringes are designed for single use only. Always follow the instructions on the package or ask your pharmacist.
Are there apps or tools that help me measure doses correctly?
Some apps can remind you when to give a dose and show a visual of the correct syringe level, but they don’t replace the physical syringe. Augmented reality dose verification tools are being tested in hospitals, but they’re not yet available to the public. The best tool is still a simple, clear oral syringe with mL markings. Use that, and double-check the label.
What should I do if I think I gave the wrong dose?
Call your pharmacist or doctor immediately. Don’t wait for symptoms. Even if your child seems fine, an overdose can take hours to show up. Keep the medicine bottle and syringe handy so you can tell them exactly what you gave. It’s better to be safe than sorry.
