Medications That Are High-Risk for Seniors: What to Review
 Dec, 1 2025
Dec, 1 2025
Every year, thousands of seniors end up in the hospital-not because of a fall, infection, or heart problem-but because of a medication they were told to take. It’s not rare. It’s not an accident. It’s a pattern. And it’s preventable.
If you or someone you love is over 65 and taking five or more pills a day, you’re not alone. About 40% of older adults in the U.S. are doing the same. But here’s the hard truth: some of those pills might be doing more harm than good. The Beers Criteria, updated in 2023 by the American Geriatrics Society, is the gold standard for spotting which medications are risky for seniors. It’s not a suggestion. It’s a warning. And if your doctor hasn’t reviewed your meds against it, you’re flying blind.
What Makes a Medication High-Risk for Seniors?
It’s not about the drug being dangerous for everyone. It’s about how aging changes the body. As we get older, our kidneys slow down. Our liver doesn’t break down drugs as fast. Our brains become more sensitive to sedatives. And that changes everything.
Take zolpidem (Ambien®). It’s a common sleep aid. But in seniors, it lingers in the system-up to 11 hours after taking it. That’s why 2.5 times more older adults who take it fall and break hips. Sleepwalking, confusion, dizziness-these aren’t side effects you can ignore. They’re red flags.
Then there’s glyburide (Diabeta®), a diabetes pill. It’s cheap. It’s old. And it’s dangerous for seniors. While younger people can handle it, older adults have a 29.3% chance of dropping their blood sugar so low they end up in the ER. That’s nearly three times higher than with glipizide, a safer alternative. The FDA even added a boxed warning in 2023-clearly saying: avoid this in people over 65.
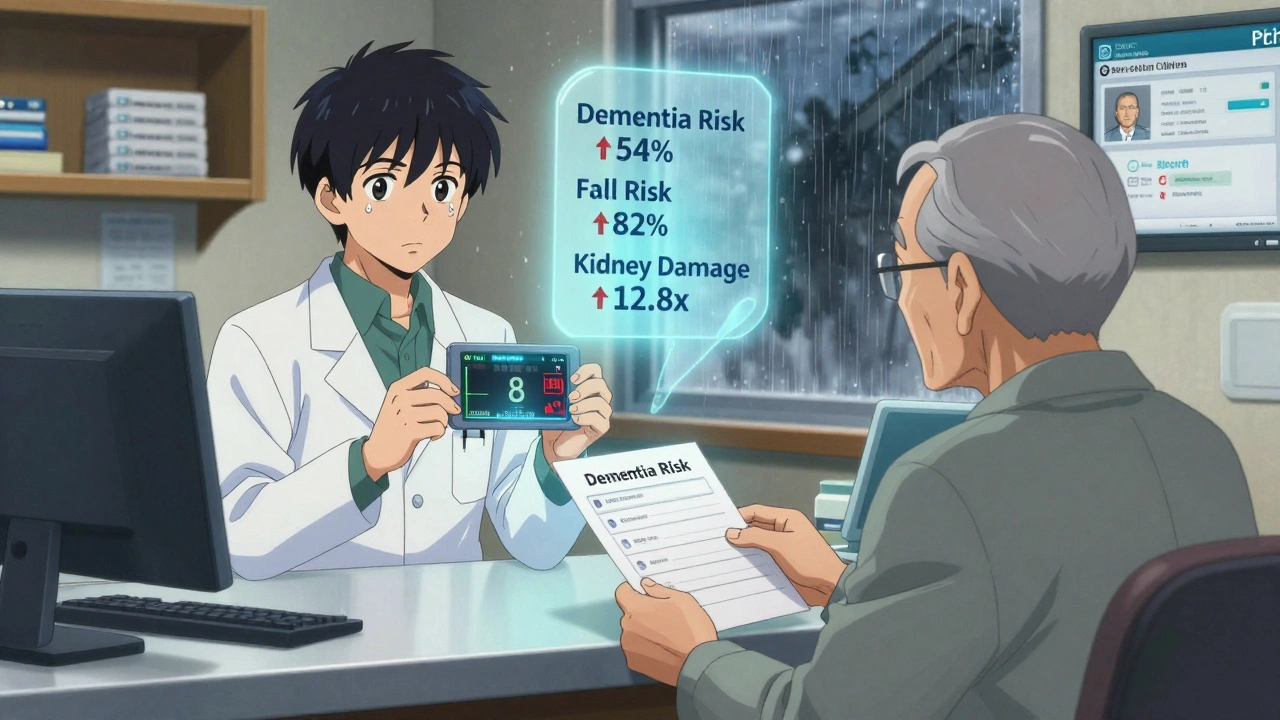
Anticholinergic drugs are another silent killer. These include diphenhydramine (Benadryl®), amitriptyline (Elavil®), and promethazine (Phenergan®). They block a brain chemical called acetylcholine. Sounds harmless, right? But in seniors, that leads to memory loss, confusion, constipation, and even a 54% higher risk of dementia after just three years of use. One study found that taking these drugs for more than 1,095 days-about three years-doubles the odds of developing Alzheimer’s.
And don’t forget nitrofurantoin (Macrobid®), often prescribed for UTIs. It’s fine for younger people. But if your kidneys aren’t working perfectly-common in seniors-it can cause deadly lung damage. The risk? 12.8 times higher if your kidney filter rate is below 60. And when it happens, nearly 1 in 5 people don’t survive.
The Top 5 High-Risk Medications to Review Now
These aren’t hypotheticals. These are real drugs, prescribed every day, that are putting seniors at serious risk. Here’s what to look for:
- Zolpidem (Ambien®, Zolpimist) - Sleep aid. Increases fall risk by 82%. Residual drowsiness lasts hours. Avoid in anyone over 65. Safer alternatives: trazodone, cognitive behavioral therapy for insomnia (CBT-I).
- Glyburide (Diabeta®, Glynase) - Diabetes pill. Causes severe low blood sugar. 4.2 episodes per 100 patients each year. Switch to glipizide or metformin.
- Diphenhydramine (Benadryl®, Unisom) - Allergy or sleep aid. Anticholinergic score of 3 (highest risk). Linked to dementia. Use loratadine or cetirizine instead.
- Promethazine (Phenergan®) - Nausea and allergy drug. Causes extreme drowsiness, tremors, and seizures in seniors with Parkinson’s or epilepsy. Ondansetron is safer.
- Benzodiazepines (Lorazepam, Diazepam, Alprazolam) - Anxiety and sleep meds. Increase fall risk by 50%. Risk of death over five years goes up. Try non-drug options first: mindfulness, light exercise, sleep hygiene.
These five alone account for over 60% of preventable hospitalizations related to medications in seniors. And they’re all still being prescribed-often because no one asked if they were still needed.
Why Doctors Keep Prescribing Them
You might wonder: if these drugs are so risky, why are they still on the shelf? The answer isn’t malice. It’s inertia.
Many doctors were trained to prescribe these drugs decades ago. They’re familiar. They’re cheap. And if a patient says, “I can’t sleep,” it’s easier to write a script than to spend 20 minutes talking about sleep hygiene, caffeine, or anxiety.
Also, many seniors see multiple doctors. One prescribes a sleep aid. Another adds an antihistamine for allergies. A third gives a muscle relaxant. No one sees the full picture. That’s polypharmacy-the danger of too many pills stacking up. It’s not just the drugs themselves. It’s how they interact.
For example, combining ciprofloxacin (an antibiotic) with warfarin (a blood thinner) can spike INR levels by 47%. That means a higher chance of internal bleeding. One patient I know was on both. She started bruising easily. Her doctor didn’t connect the dots until she ended up in the ER with a bleeding ulcer.
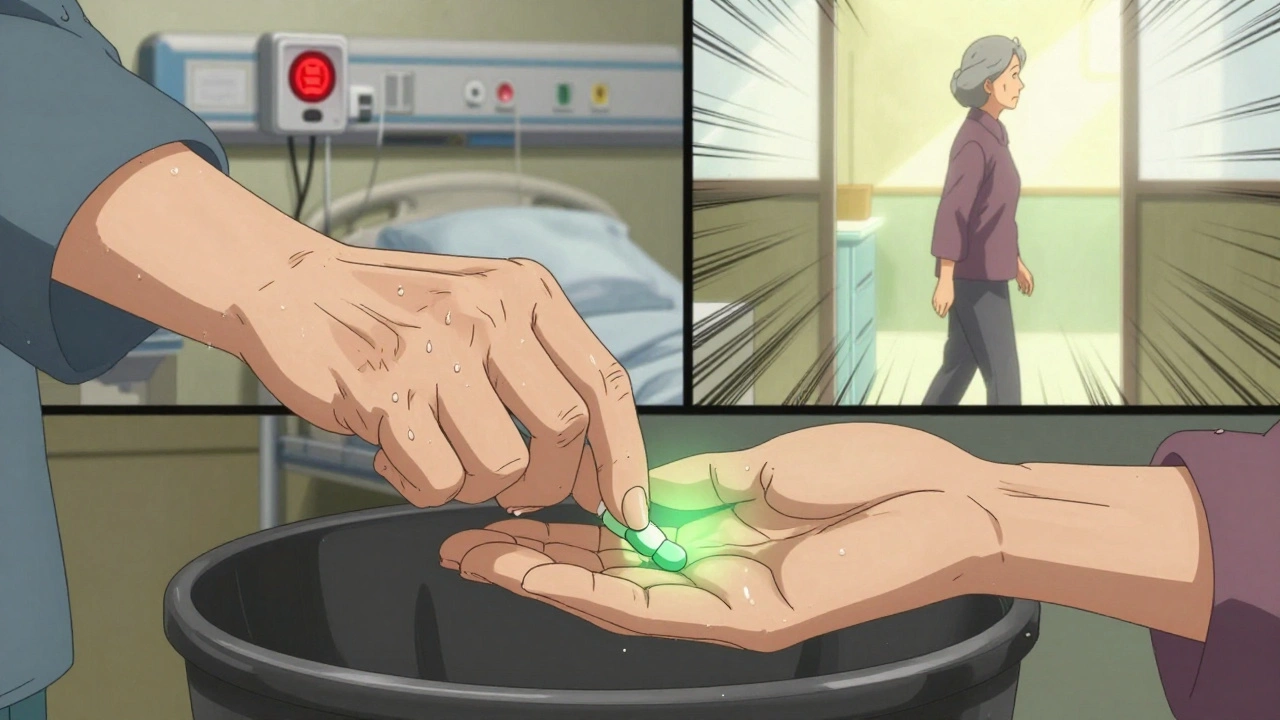
What You Can Do: The Brown Bag Review
You don’t need to be a doctor to protect yourself or a loved one. Here’s how to start:
- Collect every pill, vitamin, supplement, and OTC medicine you take. Put them in a brown bag.
- Bring them to your doctor or pharmacist. Say: “I want to review every one of these. Are any of them risky for someone my age?”
- Ask: “Is this still necessary? Can we try something safer? What happens if I stop this?”
- Request an Anticholinergic Burden Score. If it’s above 3, you’re in danger zone.
- Ask for a medication list update. Keep it in your wallet or phone.
This is called a “brown bag review.” It’s simple. It’s free. And it’s proven to cut high-risk medication use by over 30% when done by a pharmacist. Medicare even pays for it through its Medication Therapy Management program-if you’re on Part D and take multiple chronic meds.
Safer Alternatives That Actually Work
You don’t have to suffer just because a drug is risky. There are better options.
For sleep: Instead of zolpidem, try trazodone (a low-dose antidepressant with sedating effects) or CBT-I. Studies show CBT-I works better than pills for seniors-and lasts longer.
For allergies: Swap diphenhydramine for loratadine (Claritin®) or cetirizine (Zyrtec®). No drowsiness. No brain fog.
For diabetes: Glipizide or metformin replace glyburide. Both are safer. Both are just as effective.
For nausea: Ondansetron (Zofran®) is far safer than promethazine. No tremors. No seizures.
For anxiety: Don’t reach for lorazepam. Try walking, yoga, or talking therapy. If you need medicine, SSRIs like sertraline are much safer for long-term use.
For UTIs: Nitrofurantoin is risky. If your kidney function is low, ask about fosfomycin or cephalexin. Both are safer for seniors.
What’s Changing in 2025
The system is starting to wake up. In January 2024, Medicare launched a new program called “Medication Safety for Seniors.” It ties 5% of Medicare Advantage plan payments to how well they reduce high-risk prescriptions. That means insurers now have a financial reason to push doctors to switch meds.
Electronic health records like Epic and Cerner now automatically flag Beers Criteria drugs when a doctor tries to prescribe them to someone over 65. If you’re on a modern system, your doctor should see a warning pop up.
And pharmacies? Most now use tools like Surescripts that check your meds in real time. If you’re on a risky combo, the pharmacist can call your doctor before filling it.
This isn’t perfect. But it’s progress. And it means you have more power than you think.
When to Say No-and How to Do It
Sometimes, you’ll be told: “This is the only option.” That’s not true.
Here’s what to say:
- “I’ve read this might be risky for seniors. Is there a safer alternative?”
- “Can we try stopping this for a few weeks and see how I feel?”
- “I’m worried about falls. Is this contributing to that?”
- “Can we schedule a medication review with a pharmacist?”
Doctors want to help. But they’re busy. You have to speak up. You’re not being difficult. You’re being smart.
And if your doctor resists? Get a second opinion. Go to a geriatrician. Ask for a medication therapy management session. These services exist for a reason.
Final Thought: Your Meds Are Not Set in Stone
Medications aren’t tattoos. They’re tools. And tools can be swapped out when they’re no longer safe.
If you’re taking five or more pills, chances are at least one of them could be replaced-or removed-without hurting your health. Maybe even improving it.
Don’t wait for a fall. Don’t wait for confusion. Don’t wait for a hospital stay. Start today. Grab your brown bag. Make the call. Ask the questions.
Because the best medicine for seniors isn’t always a pill. Sometimes, it’s the courage to ask: ‘Do I really need this?’
What is the Beers Criteria and why does it matter for seniors?
The Beers Criteria is a list of medications that are potentially unsafe for adults over 65, updated every two years by the American Geriatrics Society. It’s based on decades of research showing which drugs increase fall risk, confusion, kidney damage, or dementia in older adults. It matters because over 40% of seniors take five or more medications, and many of those are on this high-risk list. Medicare and most health plans use it to guide prescribing and coverage decisions.
Can I just stop taking a high-risk medication if I’m worried?
No. Stopping suddenly can be dangerous, especially with drugs like benzodiazepines, sleep aids, or antidepressants. Withdrawal can cause seizures, rebound insomnia, or severe anxiety. Always talk to your doctor first. They can help you taper off safely, usually over 4-6 weeks. Never stop cold turkey.
Are over-the-counter drugs like Benadryl really risky for seniors?
Yes. Diphenhydramine (Benadryl®) is one of the most dangerous OTC drugs for seniors. It’s a strong anticholinergic, meaning it blocks brain chemicals needed for memory and focus. Studies show taking it for more than three years increases dementia risk by 54%. It also causes dizziness, constipation, and urinary retention. Safer options include loratadine (Claritin®) or cetirizine (Zyrtec®).
How often should seniors have their medications reviewed?
At least once a year, but every 3-6 months is better if you’re taking five or more medications. If you’ve recently been hospitalized, had a fall, or started seeing a new doctor, get a review right away. Medicare covers an annual medication therapy management session for seniors on multiple chronic meds.
What should I bring to a medication review appointment?
Bring all your medications in a brown bag: prescription pills, vitamins, supplements, OTC drugs, and even herbal remedies. Include the names, dosages, and how often you take them. If you have a list from your pharmacy, bring that too. The more complete your list, the better your doctor or pharmacist can spot problems.
Can a pharmacist help me with my medication review?
Yes, and they often know more than your doctor about drug interactions. Pharmacists are trained to spot high-risk combinations and can recommend safer alternatives. Many pharmacies offer free medication reviews. Medicare also pays for Medication Therapy Management (MTM) services if you’re on multiple chronic medications. Ask your pharmacist if you qualify.

sagar bhute
December 3, 2025 AT 10:55This article is pure alarmism. People have been taking these meds for decades without issue. If you're too frail to handle glyburide, maybe you shouldn't be living alone. Stop coddling the elderly and start teaching them responsibility.
Cindy Lopez
December 4, 2025 AT 17:00There is no such thing as a 'safe' alternative to zolpidem. Trazodone is not FDA-approved for insomnia. CBT-I is a luxury most seniors can't access. This article ignores reality.
Francine Phillips
December 6, 2025 AT 01:04I know someone who died from a fall after switching from Ambien to trazodone. The dizziness was worse. I'm not convinced this is better.
Katherine Gianelli
December 7, 2025 AT 21:44To anyone scared by this list - you're not alone. I helped my mom go through her brown bag last year. We cut out three meds, kept two that were actually helping, and she’s sleeping better, walking steadier, and actually remembering where she put her glasses. It wasn’t easy. But it was worth it. You don’t have to do it alone. Ask for help. Ask your pharmacist. They’re the real heroes here.
Makenzie Keely
December 9, 2025 AT 06:34PLEASE SHARE THIS WITH EVERY SENIOR YOU KNOW! And if you’re a caregiver - print it out. Tape it to the fridge. Bring it to the doctor. This isn’t fear-mongering - it’s life-saving. I’ve seen too many grandmas on Benadryl because it’s ‘cheap’ and ‘easy.’ It’s not. It’s poisoning their brains slowly. Loratadine costs $4 at Walmart. Why are we still doing this?!
Jim Schultz
December 10, 2025 AT 18:32Oh, here we go - the Beers Criteria again. The same list that’s been used since 2012. And yet, every single one of these drugs is still in the top 100 prescribed to seniors. Why? Because the FDA doesn’t ban them. Because insurance companies still cover them. Because doctors are too lazy to re-educate themselves. And because, let’s be honest - if you’re 82 and your hip hurts, you don’t care about dementia risk in 2030. You want to sleep. You want to not itch. You want to not feel like you’re dying. This isn’t a medical issue - it’s a societal failure. And you? You’re just yelling into the void.
Ignacio Pacheco
December 11, 2025 AT 00:32So… we’re supposed to stop giving seniors sleep aids because they might fall? What’s the alternative? Let them lie awake for 8 hours screaming at the ceiling? And then we wonder why they’re depressed? This isn’t medicine - it’s moralizing with a clipboard.
Charles Moore
December 11, 2025 AT 17:20I’m from Ireland, and we’ve had a similar problem here. Our geriatricians started pushing for mandatory med reviews after a spike in falls. It’s not about taking meds away - it’s about replacing them with something that actually fits the body you have now, not the one you had in 1985. I’ve seen it work. It’s not perfect, but it’s better than pretending nothing’s changed.
Joykrishna Banerjee
December 13, 2025 AT 06:52Let me be clear: the Beers Criteria is a Marxist-inspired tool designed to ration care for the elderly. It’s not science - it’s ideology dressed in clinical jargon. The real problem? Overpopulation. Underfunded hospitals. And the fact that nobody wants to admit that aging is a burden. We’re not ‘reviewing meds’ - we’re quietly euthanizing the elderly with bureaucratic indifference.
Kara Bysterbusch
December 13, 2025 AT 08:09As someone who spent 18 months coordinating care for my mother - who was on 11 medications, including diphenhydramine for ‘allergies’ and nitrofurantoin despite an eGFR of 42 - I can say with absolute certainty: this article saved her life. We removed three drugs, reduced two, and added a daily walk. Her confusion lifted. Her appetite returned. She started reading again. She didn’t need more pills. She needed someone who knew how to listen. The brown bag review? It’s not a gimmick. It’s a lifeline. And if your doctor doesn’t offer it - ask until they do. Because your life - or your mother’s, your father’s, your aunt’s - is not a statistic. It’s a person.
Vincent Soldja
December 14, 2025 AT 09:09Agreed. The Beers Criteria is outdated. Many drugs on the list are still first-line in Europe. This is American medical exceptionalism at its worst. Also, CBT-I is inaccessible to 90% of rural seniors. The real solution? Better training for primary care physicians. Not fear.