Metabolic Surgery Outcomes: Real Weight Loss and Diabetes Remission Results
 Jan, 12 2026
Jan, 12 2026
When someone has type 2 diabetes and obesity, losing weight isn’t just about fitting into smaller clothes. It’s about reversing a disease that’s slowly damaging their heart, kidneys, nerves, and eyes. For many, diet and pills just don’t cut it. That’s where metabolic surgery comes in - not as a last resort, but as one of the most powerful tools we have to truly change the course of diabetes.
What Metabolic Surgery Actually Does
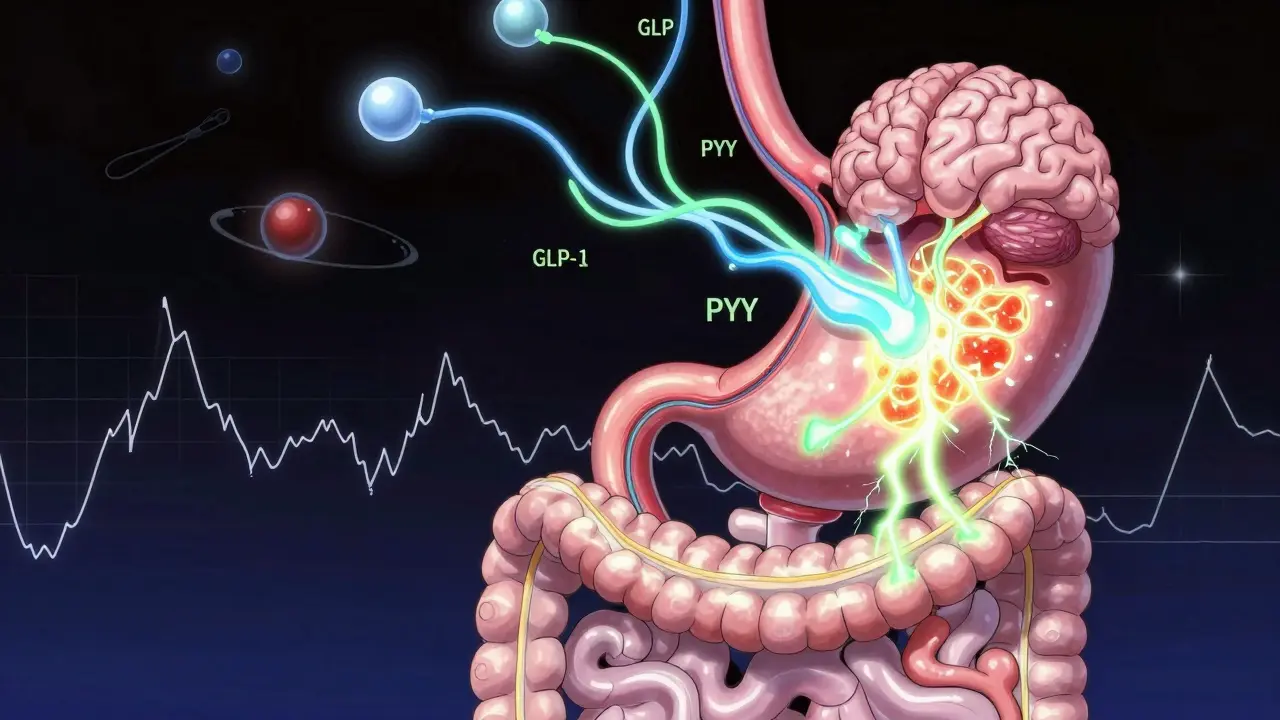
Metabolic surgery isn’t just about shrinking your stomach. It’s about rewiring how your body handles food, blood sugar, and hunger. These procedures - like gastric bypass, sleeve gastrectomy, and duodenal switch - change the anatomy of your digestive system. And that change sends new signals to your brain, pancreas, and liver.Here’s the surprising part: blood sugar levels often drop within days after surgery - long before you’ve lost much weight. That’s because the surgery alters gut hormones like GLP-1 and PYY, which tell your body when to release insulin and when to feel full. This isn’t just weight loss. It’s metabolic reset.
How Much Weight Do People Really Lose?
Numbers matter. A 2024 study in JAMA followed people with severe obesity (average BMI of 45.9) for six years. Those who had gastric bypass lost nearly 20% of their total body weight. Those who stuck with diet and medication? Less than 9%. That’s more than double the difference.Another study found that patients lost an average of 27.7% of their starting weight after surgery. Compare that to the 0.2% lost by people on medical therapy alone. These aren’t small gains. For someone weighing 250 pounds, that’s over 69 pounds gone - and most of it stays off.
When you look at excess weight loss - meaning weight lost beyond what’s considered healthy for their height - gastric bypass patients average 55% loss. Sleeve gastrectomy patients lose about 50%. That’s not just weight. That’s a new life.
Diabetes Remission: The Real Win
Remission doesn’t mean cured. It means no more diabetes meds, normal blood sugar, and HbA1c below 6.5% without drugs. And metabolic surgery delivers that more than anything else.The Swedish Obese Subjects study tracked patients for 15 years. After surgery, 30.4% stayed in remission. In the non-surgical group? Just 6.5%. That’s nearly five times higher.
One-year remission rates vary by procedure:
- Biliopancreatic diversion/duodenal switch: 95.1%
- Gastric bypass: 80.3%
- Sleeve gastrectomy: 75.6%
- Gastric banding: 56.7%
Even five years later, gastric bypass patients still had a 29% chance of being off all diabetes meds. Sleeve gastrectomy held at 23%. That’s better than any pill on the market.
Who Benefits the Most?
Not everyone responds the same. The best candidates have:- Been diagnosed with type 2 diabetes for less than 10 years
- Don’t need insulin (or have been on it for less than a year)
- Still produce some of their own insulin
- Have a BMI of 30 or higher - even if they’re not severely obese
Studies show patients with BMIs between 24 and 30 - who are overweight, not obese - still had a 93% remission rate after gastric bypass. That’s huge. It means surgery isn’t just for people with extreme weight problems.
Insulin users? Their remission rate drops. Why? Because their pancreas has been working too hard for too long. Once beta cells burn out, even surgery can’t fully bring them back. But even then, most still need fewer pills and lower doses.
What Happens After the First Year?
The early wins are impressive. But what lasts? That’s the real question.Five years after surgery, about 1 in 3 patients still have full remission. Another 1 in 4 have partial remission - meaning their blood sugar is better, but they still need a little medication. Only 1 in 5 relapse completely.
That’s still better than medical therapy. In the ARMMS-T2D trial, only 6.2% of people on diet and drugs had remission at seven years. Surgery? 18.2%.
But here’s the catch: remission can fade. Weight regain, aging, and ongoing beta cell decline can bring diabetes back. That’s why follow-up isn’t optional. It’s essential. Regular blood tests, nutrition checks, and lifestyle support keep the benefits alive.
The Hidden Benefits Beyond Blood Sugar
Metabolic surgery doesn’t just fix diabetes. It fixes the whole metabolic mess.At seven years, patients had:
- Higher HDL (good cholesterol)
- Lower triglycerides
- Lower blood pressure
- Less fatty liver
One study found that for every year someone stayed in remission, their risk of kidney disease, nerve damage, and eye problems dropped by 19%. That’s not just feeling better. That’s living longer.
The Risks Are Real - But Manageable
No surgery is risk-free. After metabolic surgery, you might face:- Nutritional deficiencies (iron, B12, vitamin D, calcium)
- Anemia
- Bone fractures (due to reduced calcium absorption)
- Dumping syndrome (nausea, cramps after sugary foods)
- Need for lifelong supplements and blood tests
These aren’t deal-breakers. They’re responsibilities. Patients who stick with their follow-up care - taking supplements, seeing their dietitian, getting labs done - rarely have serious problems. The real danger is skipping care because you feel fine.
Who Should Consider It?
Guidelines say metabolic surgery is recommended for:- People with BMI ≥40, with or without diabetes
- People with BMI 35-39.9 and uncontrolled diabetes despite medication
- People with BMI 30-34.9 and diabetes that won’t respond to pills or diet
That last group is new. Five years ago, insurance wouldn’t cover it. Now, more providers are recognizing that diabetes can be reversed - even in people who aren’t severely obese.
Before surgery, you’ll need:
- At least 6 months of documented medical management failure
- A psychological evaluation
- Nutritional counseling
- Commitment to lifelong follow-up
Why Isn’t Everyone Getting It?
Less than 2% of eligible people in the U.S. get metabolic surgery each year. Why?- Insurance won’t cover it for BMI under 35
- Doctors don’t bring it up
- Patients fear surgery
- People think it’s a “cop-out” - not a real solution
But here’s the truth: if a pill could give you 80% remission, drop your HbA1c from 9.5 to 5.8, and cut your risk of amputation by half - you’d take it. Surgery is that pill. It’s just more invasive.
What About Non-Surgical Options?
New tools like the intragastric balloon and AspireAssist offer weight loss without cutting. The DiRECT trial showed that a very low-calorie diet could get 46% of people into remission at one year. That’s impressive.But here’s the catch: most people regain the weight within a year or two. Surgery? The results last. It’s not about which is better. It’s about which fits your life. Surgery requires commitment. So does diet. But surgery changes your biology - diet only changes your behavior.
Final Thoughts: It’s Not a Miracle. It’s a Tool.
Metabolic surgery won’t fix everything. You still need to eat well. Move your body. Sleep. Manage stress. But it gives you a massive head start. It breaks the cycle of hunger, insulin resistance, and weight gain that pills can’t touch.If you’ve been told you’ll have diabetes for life - and you’ve tried everything - surgery might not be the end of the road. It might be the beginning of a new one.
Can metabolic surgery cure type 2 diabetes?
No, it doesn’t cure diabetes. But it can put it into remission - meaning you stop taking medication and your blood sugar stays normal without drugs. For many, this lasts years. Some stay in remission for over a decade. But it’s not permanent for everyone. Weight regain or long-term beta cell decline can bring diabetes back. That’s why lifelong monitoring is critical.
Which metabolic surgery has the best diabetes remission rate?
Biliopancreatic diversion with duodenal switch has the highest one-year remission rate at 95.1%. Gastric bypass follows closely at 80.3%. Sleeve gastrectomy is effective too, with 75.6% remission at one year. But each procedure has different risks and long-term needs. Duodenal switch requires more lifelong supplements. Gastric bypass has more proven long-term data. The best choice depends on your health, BMI, and willingness to stick with follow-up care.
Can you have metabolic surgery if you’re not obese?
Yes. Studies now show that people with BMI as low as 24-30 - who are overweight, not obese - can still achieve over 90% diabetes remission after gastric bypass. The American Diabetes Association and other groups now support surgery for patients with BMI 30-34.9 if their diabetes is uncontrolled. The key isn’t how much you weigh - it’s whether your body can’t manage blood sugar with other methods.
How long does it take to see results after surgery?
Blood sugar often drops within days - sometimes even before you lose significant weight. That’s because the surgery changes gut hormones that control insulin. Most people stop taking diabetes meds within weeks. Weight loss starts fast - up to 5-10 pounds a month in the first few months - and slows after 12-18 months. Full remission is usually confirmed by six months to one year after surgery.
What are the biggest risks after metabolic surgery?
The biggest long-term risks are nutritional: low iron, vitamin B12, vitamin D, and calcium. This can lead to anemia, bone loss, and fractures. Other common issues include dumping syndrome (feeling sick after sugar), nausea, and changes in bowel habits. These aren’t rare - but they’re preventable. Taking prescribed supplements, getting regular blood tests, and seeing your dietitian every 3-6 months cuts these risks dramatically. The real danger isn’t the surgery - it’s skipping follow-up.

John Tran
January 12, 2026 AT 23:56So let me get this straight-this surgery doesn’t just shrink your stomach, it rewires your soul? Like, you press a button and suddenly your body stops craving donuts and starts chanting affirmations to your pancreas? I mean, I get it, science is magic now, but why does it feel like we’re just replacing one addiction (sugar) with another (surgical salvation)? I’ve seen people post before-and-after pics like they won the lottery, but nobody talks about the 3 a.m. panic attacks when they realize they can’t eat pizza anymore… or that their spouse now treats them like a fragile porcelain doll because ‘you had surgery, you’re different.’ This isn’t a reset-it’s a reboot with a side of existential dread. And don’t even get me started on the supplements. I’m supposed to take 17 pills a day like I’m a dragon hoarding vitamins? I’d rather just eat the damn donut and die happy.
mike swinchoski
January 13, 2026 AT 07:55You people are so lazy. You want a quick fix. You don’t want to work. Just eat less and move more. That’s it. No magic. No surgery. Just discipline. You think your body is some broken machine that needs a mechanic? It’s not. It’s just weak. Stop blaming your genes. Stop blaming your hormones. You just need to try harder. I lost 80 pounds with just walking and water. No knives. No pills. Just willpower. If you can’t do that, you don’t deserve to be healthy.
jefferson fernandes
January 14, 2026 AT 06:07Mike, I hear you-but you’re oversimplifying. This isn’t about laziness; it’s about biology. Type 2 diabetes isn’t a moral failure-it’s a metabolic disorder. And yes, willpower matters, but when your brain is flooded with ghrelin and your pancreas is screaming for mercy, willpower is like trying to hold back a tsunami with a toothpick. Metabolic surgery doesn’t remove willpower-it removes the biological barriers to it. People who’ve tried every diet, every pill, every cleanse, and still couldn’t get their HbA1c below 8? They’re not weak. They’re trapped. Surgery gives them a door out. And yes, it’s not perfect. But neither is forcing someone to starve themselves for life while their kidneys slowly fail. Let’s stop shaming and start solving.
Acacia Hendrix
January 14, 2026 AT 18:38Frankly, the data is compelling, but the framing remains dangerously reductive. The notion of 'remission' as a binary outcome-either you're cured or you're not-ignores the dynamic nature of metabolic homeostasis. The gut-brain axis modulation via altered enteroendocrine signaling is not merely hormonal; it's epigenetic. The sustained downregulation of inflammatory cytokines post-sleeve gastrectomy, for instance, correlates with improved adipokine profiles, which in turn modulate insulin sensitivity independently of weight loss. We're not just talking about a 'reset'-we're witnessing a phenotypic reprogramming. And yet, the discourse remains stuck in the 1990s: 'lose weight, cure diabetes.' The nuance is being erased by pop-science soundbites.
James Castner
January 16, 2026 AT 15:09Let me say this with all the gravity and respect this subject deserves: we are standing at the precipice of a medical revolution-and we are still arguing over whether to turn on the light. Metabolic surgery is not a ‘cop-out.’ It is the most profound, scientifically validated intervention we have ever developed to reverse a chronic, systemic, life-stealing disease. We do not tell a heart attack survivor, ‘Just eat less butter,’ we do angioplasty. We do not tell a cancer patient, ‘Try harder not to have tumors,’ we remove them. So why, in the case of diabetes, do we insist that the body’s failure is somehow a personal failure? The data is not ambiguous. The outcomes are not marginal. The life expectancy gains? The reduction in amputations, dialysis, blindness? These are not statistics-they are human beings getting their lives back. And if we continue to let insurance companies and stigma dictate who gets access to this, we are not just negligent-we are cruel.
Adam Rivera
January 17, 2026 AT 13:41Hey, I just wanted to say thanks for writing this. My cousin had the bypass last year-she was on insulin, couldn’t walk up the stairs, felt like she was dying slowly. Now? She’s hiking, playing with her kids, eating pizza once a week (yes, she still eats pizza). She still takes her vitamins, still goes to checkups, still has to be careful-but she’s alive again. I used to think surgery was for people who couldn’t control themselves. Now I know it’s for people who tried everything and still got crushed by their own bodies. I’m telling everyone I know about this. We need more stories like this. Not just numbers. Real people.
Rosalee Vanness
January 17, 2026 AT 20:22I’ve been on the other side of this-diagnosed at 28, tried every diet, every app, every ‘miracle tea,’ every trainer who promised results. I lost 40 pounds twice… and gained it all back twice. I cried in the grocery store because I couldn’t even buy a bagel without feeling like a failure. Then I had the sleeve. It wasn’t magic-it was a second chance. The first week, I didn’t even think about food. I just… breathed. And then came the slow, quiet work: learning to eat again, not like a machine, but like a human who finally has space to heal. I still have days where I miss cookies. But now I have tools. I have a team. I have bloodwork that doesn’t make my doctor sigh. And I have a life that doesn’t revolve around my next meal. If you’re reading this and you’re tired… please, don’t give up. Surgery isn’t the end of your journey-it’s the beginning of the one you were meant to live.
lucy cooke
January 18, 2026 AT 02:28Oh please. Let’s not pretend this is some noble, revolutionary breakthrough. It’s just the latest capitalist fantasy dressed in lab coats: ‘Buy this procedure, become a better version of yourself!’ Meanwhile, the real issue-the food industry, the agricultural subsidies, the systemic poverty that makes processed carbs cheaper than kale-is ignored. You think people don’t know they’re sick? They do. But they’re also exhausted, overworked, underpaid, and told daily that their bodies are the problem, not the system. Surgery is a Band-Aid on a gunshot wound. And now we’re selling it as the cure? How convenient for the hospitals. How tragic for the people who can’t afford it-or worse, who can’t even get their doctor to mention it because ‘you’re not obese enough.’ This isn’t progress. It’s performance.