Noninvasive Liver Fibrosis Tests: FibroScan and Serum Scores Explained
 Jan, 30 2026
Jan, 30 2026
Why Liver Fibrosis Testing Matters More Than Ever
More than 1 in 4 adults worldwide have fatty liver disease, and for about 1 in 5 of them, it’s turning into something more dangerous: liver scarring, or fibrosis. Left unchecked, this can lead to cirrhosis, liver failure, or even cancer. The old way to check for fibrosis-inserting a needle into the liver to take a tissue sample-is risky, painful, and often inaccurate because of sampling errors. That’s why doctors now rely on noninvasive tests like FibroScan and blood-based scores such as FIB-4, APRI, and ELF. These tools let you know if your liver is scarred without a single incision.
How FibroScan Works: The Ultrasound That Feels Like a Bounce
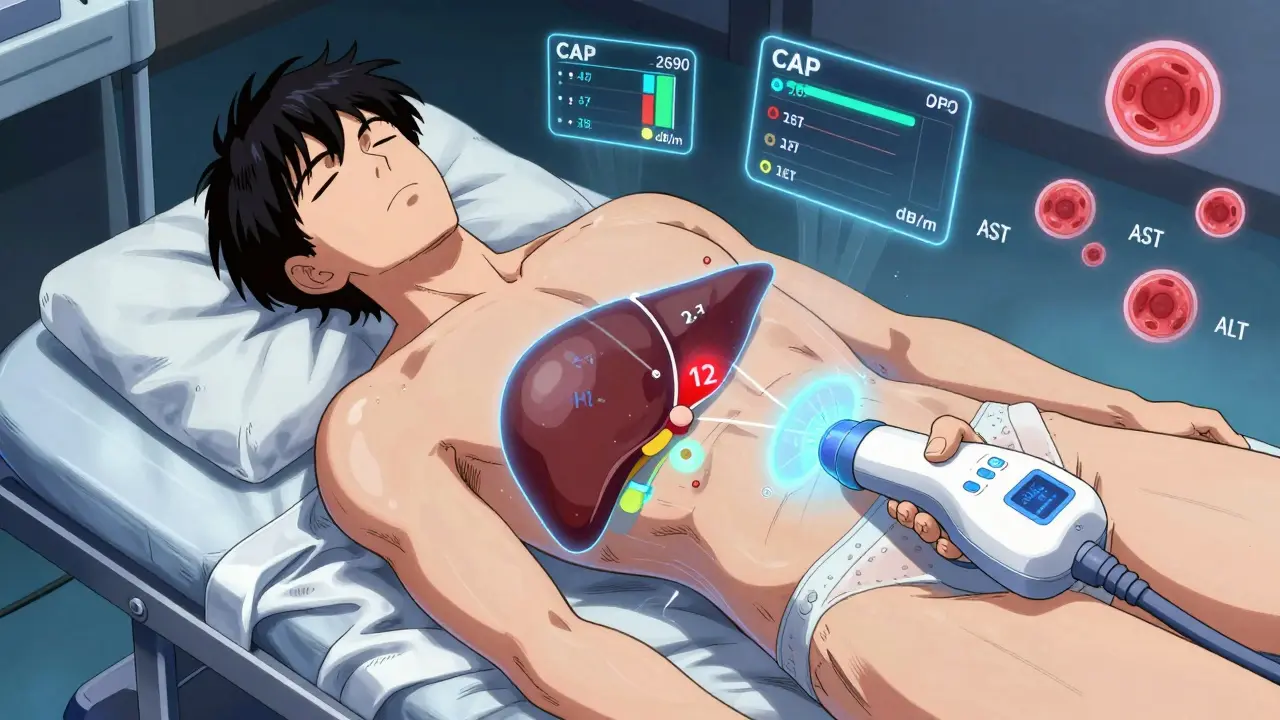
FibroScan isn’t a traditional ultrasound. It’s a handheld device that sends a gentle pulse of low-frequency waves through your skin and into your liver. These waves move faster when the liver is stiff from scarring. The machine measures how fast they travel and gives you a number in kilopascals (kPa). A normal liver reads between 2 and 7 kPa. Above 7 kPa? That’s a red flag. Above 12 kPa? It’s likely advanced fibrosis or cirrhosis.
The device uses two probes: the S probe for most people, and the XL probe for those with higher body weight or more fat in the liver. If you have a BMI over 28 or a CAP score above 268 dB/m, your provider should use the XL probe. Without it, the test might fail-or give you a false reading. In fact, about 1 in 10 tests don’t work on the first try, especially in people with obesity. One patient on Reddit said he had to try three times before the XL probe finally worked, adding $200 to his bill.
What the CAP Score Tells You About Fat in Your Liver
FibroScan doesn’t just measure stiffness. It also measures fat-called the Controlled Attenuation Parameter, or CAP. CAP scores range from 100 to 400 dB/m. Here’s what they mean:
- 238-260 dB/m: 11-33% fat in your liver
- 260-290 dB/m: 34-66% fat
- 290-400 dB/m: 67% or more fat
But here’s the catch: CAP overpredicts fat in obese people. A study from Duke University found that 81% of patients with mild fat on biopsy were flagged as having severe fat by CAP. That means the test might scare you unnecessarily if you’re overweight. It’s a useful tool, but not perfect.
Serum Scores: Blood Tests That Predict Scarring
Instead of a machine, serum scores use routine blood tests you’ve probably already had: AST, ALT, platelet count, and sometimes glucose. The most common ones are FIB-4, APRI, and ELF.
FIB-4 uses your age, AST, ALT, and platelets. If your score is below 1.3, you’re very unlikely to have advanced fibrosis. That’s a powerful rule-out tool. If it’s above 2.67, you’re at high risk. But here’s the problem: it misses a lot of real cases. One study found it only caught 16.8% of people with advanced fibrosis. In younger people under 35, it’s even less accurate.
APRI is simpler-it only needs AST and platelets. A score over 2.0 suggests cirrhosis. It’s cheap and widely available, but not as precise as FIB-4.
ELF is more advanced. It measures three proteins in your blood that directly relate to scarring. It’s more accurate than FIB-4 or APRI, especially when they disagree. But it’s not available everywhere, and it costs more.
Which Test Is Better? It Depends on Your Situation
There’s no single best test. Each has strengths and blind spots.
FibroScan gives instant results. You walk in, get scanned, and know your liver stiffness within minutes. It’s excellent for confirming advanced fibrosis. But it fails in about 10-15% of cases, especially in obese people. It’s also expensive-$50 to $150 per test.
Serum scores like FIB-4 cost about $10. They’re built into electronic health records. One doctor in the U.S. said using FIB-4 as an automatic alert in her system raised screening rates from 12% to 67%. But you have to wait 24 to 72 hours for lab results. And they’re not great at catching early scarring.
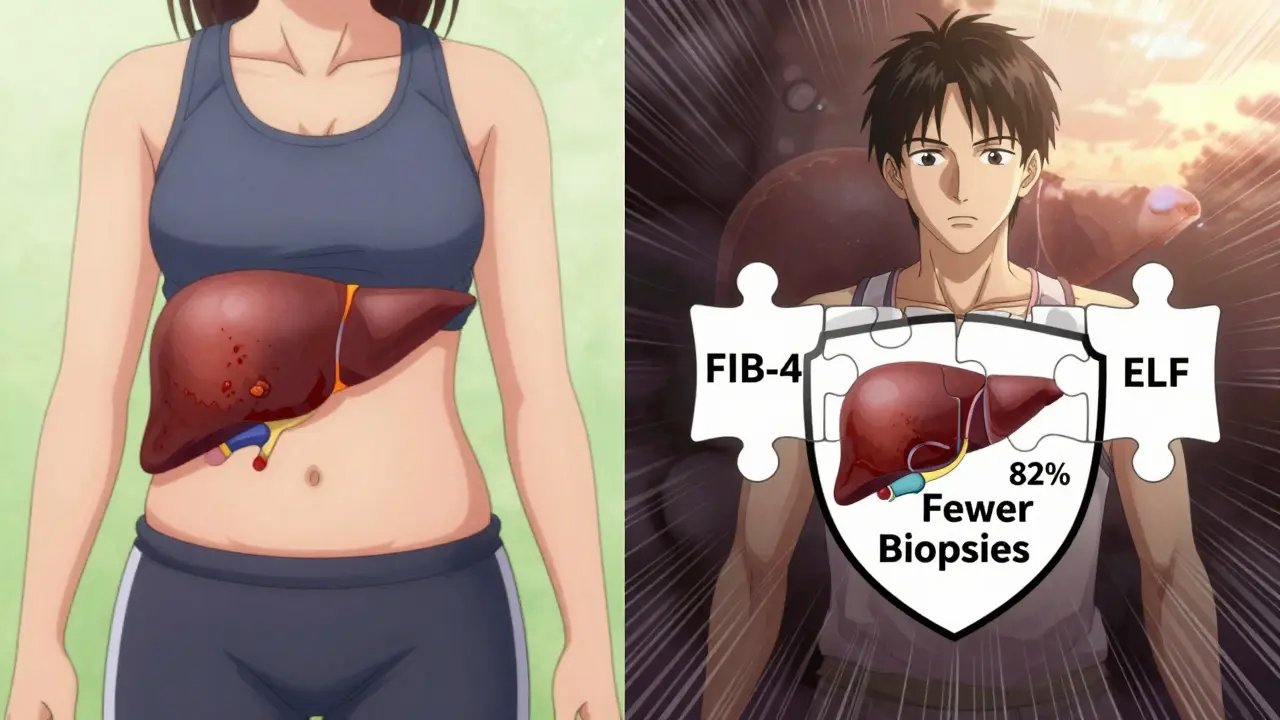
Here’s what the experts recommend: Start with FIB-4. If it’s low (<1.3), you’re probably fine. If it’s high (>2.67), move to FibroScan. If the two disagree? Use ELF or consider a biopsy. A 2020 study showed this three-step approach cuts unnecessary biopsies by 70%.
When Tests Lie: False Negatives and False Alarms
Both FibroScan and serum scores can be wrong. FibroScan can give a falsely low reading if you’ve had a recent meal, have liver inflammation (AST more than twice the normal level), or have heart failure. That’s why you’re told to fast for 3 hours before the test.
Serum scores can miss advanced fibrosis in younger people. FIB-4’s accuracy drops from 85% to 67% under age 35. It also doesn’t work well in people with autoimmune liver disease or those who’ve had hepatitis C treated with older drugs.
One patient shared a frustrating story: Her FibroScan said F2 (moderate scarring), but FIB-4 said high risk. She got a biopsy, which showed F3 (advanced). Both tests were wrong in different ways. That’s why doctors never rely on just one.
What’s New in 2026? AI, FIB-5, and Better Algorithms
The field is moving fast. In April 2024, Echosens launched FibroScan 730 with AI that predicts whether a reading is reliable. Early results show it cuts technical failures by 22%.
A new blood score called FIB-5 was introduced in 2024. It adds glucose levels to the FIB-4 formula. In diabetic patients with fatty liver, FIB-5 correctly identified advanced fibrosis in 89% of cases-better than FIB-4 alone.
Research is also testing a combined algorithm: FibroScan + FIB-4 + ELF. In a 2023 NIH trial, this trio reduced unnecessary biopsies by 82% while still catching 94% of cirrhosis cases. That’s the future: not one test, but layers of data working together.
Who Should Get Tested?
You should consider a noninvasive test if you:
- Have type 2 diabetes or obesity
- Drink alcohol regularly
- Have high cholesterol or triglycerides
- Have elevated liver enzymes on routine blood work
- Have a family history of liver disease
Even if you feel fine. Fatty liver and early fibrosis often have no symptoms. By the time you feel tired or bloated, the damage may already be advanced.
What to Do Next
If you’re at risk, ask your doctor for a FIB-4 test. It’s cheap, fast, and built into most lab systems. If your score is low, you can relax-for now. If it’s high, ask for a FibroScan. Don’t panic if the numbers don’t match. That’s normal. Bring both results to your doctor and ask: "What’s the next step?"
Most importantly: if you’re overweight or have diabetes, focus on losing weight and cutting sugar. Even a 5-10% weight loss can reverse early fibrosis. No test replaces lifestyle change.
Frequently Asked Questions
Can FibroScan detect early liver damage?
FibroScan is best at spotting advanced fibrosis (F3-F4), not early scarring (F1-F2). It can detect moderate fibrosis, but its accuracy drops significantly for mild cases. That’s why it’s often paired with FIB-4, which is better at ruling out early disease.
Is FibroScan safe for people with pacemakers?
Yes. FibroScan uses mechanical waves, not electromagnetic pulses, so it doesn’t interfere with pacemakers or other implants. It’s considered safe for nearly all patients, including pregnant women and children.
How often should I get tested for liver fibrosis?
If you’re at risk and your first test is normal, repeat it every 2-3 years. If you have fatty liver and are overweight or diabetic, annual testing is recommended. If you’ve been diagnosed with fibrosis, your doctor may want to check every 6-12 months to track progression or response to lifestyle changes.
Can I do a home version of FibroScan or FIB-4?
No. FibroScan requires a trained operator and calibrated equipment. While smartphone apps claiming to measure liver stiffness exist, none are clinically validated. FIB-4 can be calculated at home using your blood test results, but you still need a lab to run the tests. Don’t trust apps or DIY tools.
Why do some doctors still use liver biopsy?
Biopsy is still used when noninvasive tests conflict, or when there’s suspicion of another liver disease like autoimmune hepatitis or hemochromatosis. It’s also the only way to see inflammation, fat, and scarring all at once. But with modern noninvasive tools, biopsies are now needed in fewer than 20% of suspected fibrosis cases.
Final Thoughts: No Single Test, But Better Tools Than Ever
The truth is, no noninvasive test is perfect. FibroScan misses cases. Blood scores misclassify. But together, they’re powerful. The goal isn’t to find the perfect number-it’s to catch liver damage early enough to stop it. That’s why guidelines now recommend a step-by-step approach: start simple, add tools as needed, and always tie results to your overall health. If you’re at risk, don’t wait for symptoms. Ask for a FIB-4 test today. It might be the most important blood test you ever take.

Diana Dougan
January 31, 2026 AT 23:31Bobbi Van Riet
February 2, 2026 AT 20:56Kimberly Reker
February 3, 2026 AT 17:12Natasha Plebani
February 5, 2026 AT 02:13calanha nevin
February 6, 2026 AT 03:30Darren Gormley
February 7, 2026 AT 23:59Gaurav Meena
February 9, 2026 AT 21:09Kathleen Riley
February 9, 2026 AT 22:16Eliana Botelho
February 10, 2026 AT 23:17Mike Rose
February 11, 2026 AT 01:19Pawan Kumar
February 12, 2026 AT 01:25ryan Sifontes
February 13, 2026 AT 03:13