Pharmacokinetic vs Pharmacodynamic Drug Interactions Explained - A Practical Guide
 Oct, 24 2025
Oct, 24 2025
Quick Takeaways
- PK interactions change drug levels in the body; PD interactions change the drug’s effect.
- Absorption, distribution, metabolism, and excretion (ADME) drive most PK issues.
- Synergistic, additive, and antagonistic mechanisms describe PD combos.
- Therapeutic drug monitoring (TDM) helps manage PK reactions; avoidance or dose‑spacing handles many PD combos.
- New tools - pharmacogenomics, AI models, and updated FDA guidance - are reshaping how we predict and prevent both types of interactions.
What Are Pharmacokinetic and Pharmacodynamic Interactions?
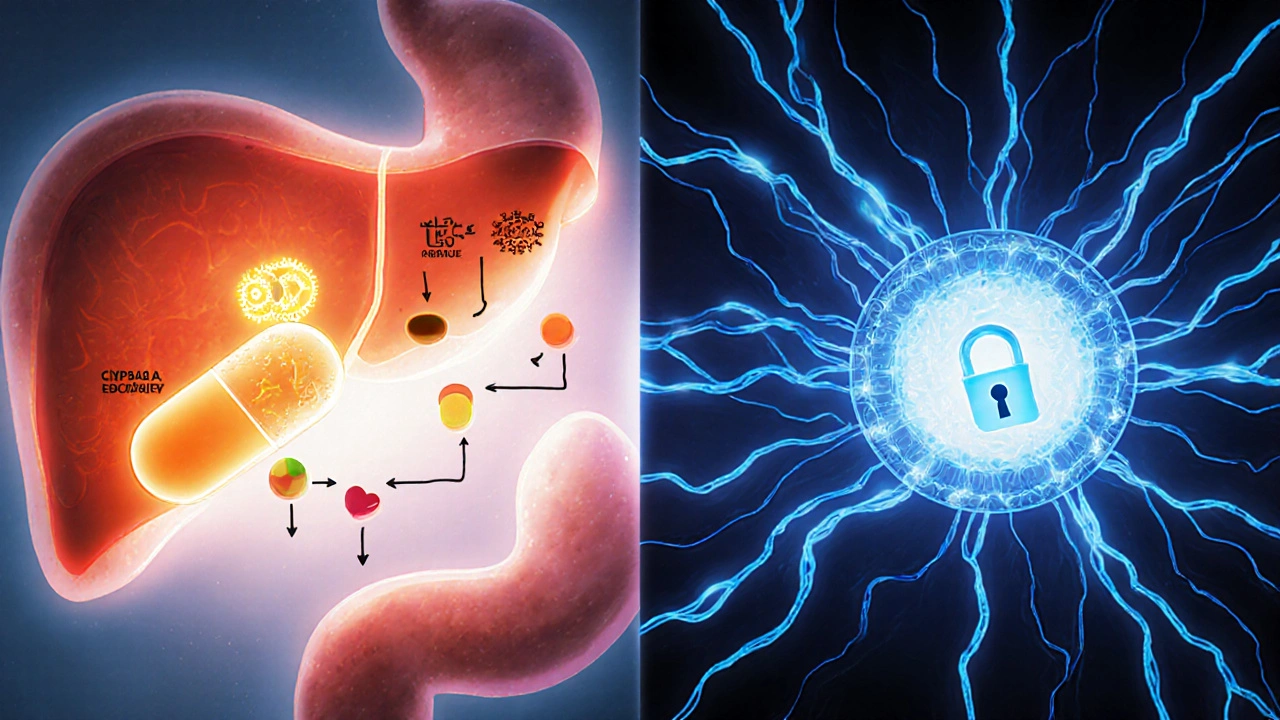
When we talk about pharmacokinetic drug interactions (PK interactions), we’re describing how the body’s handling of a medication - absorption, distribution, metabolism, or excretion - is altered by another drug. In plain language, it’s pharmacokinetic interactions that change the amount of drug that reaches the target site.
On the flip side, pharmacodynamic drug interactions (PD interactions) focus on what the drug does once it’s at the receptor. These interactions modify the drug’s effect without necessarily changing its concentration.
Both concepts were formalized in the 1950s as pharmacology split into the “what the body does to the drug” (PK) and “what the drug does to the body” (PD) frameworks. Understanding the distinction is the first step toward safer polypharmacy.
How Pharmacokinetic Interactions Occur
PK interactions can be grouped under the ADME umbrella:
- Absorption: Antacids can bind quinolone antibiotics, cutting ciprofloxacin’s uptake by 75‑90% (FDA label).
- Distribution: Phenylbutazone displaces warfarin from plasma proteins, raising free warfarin levels three‑fold (Clinical Pharmacology & Therapeutics, 1973).
- Metabolism: Clarithromycin blocks CYP3A4, causing a ten‑fold rise in simvastatin exposure (NEJM, 2004). Cytochrome P450 enzymes like CYP3A4, CYP2D6, and CYP2C9 handle about 75% of metabolism‑based interactions (Pharmacogenomics Journal, 2021).
- Excretion: Probenecid slows penicillin clearance by roughly 50% (J Pharmacol Exp Ther, 1949).
Transport proteins also matter. P‑glycoprotein‑mediated efflux accounts for 15‑20% of clinically significant PK interactions (Clinical Pharmacology & Therapeutics, 2019).
Because PK changes affect drug concentrations, they are often predictable. Therapeutic drug monitoring (TDM) - measuring plasma levels and adjusting doses - is the standard control method, especially for narrow‑therapeutic‑index drugs like warfarin, digoxin, or phenytoin.
How Pharmacodynamic Interactions Work
PD interactions hinge on how drugs influence the same physiological system. Three main patterns appear:
- Synergistic: The combined effect exceeds the sum of each drug alone. Example - sildenafil plus nitrates can cause life‑threatening hypotension.
- Additive: Effects simply add together. Warfarin plus aspirin doubles bleeding risk.
- Antagonistic: One drug blunts the other’s action. Naloxone reverses opioid analgesia.
PD interactions are harder to predict because they depend on receptor dynamics rather than serum levels. The 2023 Pharmacological Reviews paper notes that 85% of central nervous system (CNS) drug interactions are PD in nature, especially among antidepressants, antipsychotics, and opioids.
Typical PD scenarios include:
- Concurrent MAO inhibitors and SSRIs → serotonin syndrome.
- Beta‑agonist with beta‑blocker → competing receptor occupancy.
- NSAID with ACE inhibitor → reduced antihypertensive effect by 25‑30% (prostaglandin‑mediated).
Since PD combos rarely shift blood concentrations, clinicians often resort to avoiding the combination altogether rather than tweaking doses.
Clinical Impact: How Common Are These Interactions?
Adverse drug events (ADEs) represent 6.7% of UK hospital admissions (SPS, 2021). Of those, PK interactions account for about 47% and PD for 37% (Stockley’s, 12th Ed., 2022). In older adults (65+), 15% take five or more medicines daily (CDC, 2022), raising the odds of both PK and PD clashes.
High‑risk drug classes:
- PK‑heavy: Warfarin, digoxin, phenytoin - 68% of significant interactions involve PK mechanisms (UK SPS, 2023).
- PD‑heavy: Cardiovascular agents (52%) and CNS drugs (78%) (Eur J Clin Pharmacol, 2022).
Electronic health record (EHR) systems now flag thousands of interactions each month - Epic’s 2023 update listed 1,247 high‑severity PK and 983 high‑severity PD alerts based on the latest Flockhart Table.
Managing PK vs PD Interactions: Practical Strategies
PK management typically follows three steps:
- Identify the metabolic pathway (e.g., CYP3A4, CYP2D6).
- Check for known inhibitors or inducers.
- Adjust dose or monitor levels with TDM.
Example: Simvastatin 40 mg should be reduced to 10 mg when given with clarithromycin (FDA, 2016).
PD management often means:
- Map overlapping pharmacologic effects.
- Determine if additive risk is acceptable.
- If risk is high, either avoid the combo or stagger dosing times.
Clinical guidelines (NICE, 2023) suggest avoiding concurrent MAO‑I and SSRI use altogether; if unavoidable, a 14‑day washout is mandatory.
Therapeutic drug monitoring is indispensable for PK‑related drugs: the International League of Associations for TDM (2023) lists target ranges for 37 agents, including warfarin INR 2‑3 and digoxin 0.5‑2 ng/mL.
For PD combos, monitoring focuses on physiologic signs - e.g., respiratory rate <12/min for CNS depressants, INR >4.0 for additive anticoagulants, or systolic BP swings >30 mmHg for opposing cardiovascular agents (SPS, 2023).
Emerging Trends: What’s New in PK/PD Interaction Science?
Regulators are tightening requirements. The FDA’s 2023 draft guidance now mandates testing against 11 CYP enzymes and eight transporters, up from seven in 2017. This pushes drug developers to generate richer interaction data early.
Pharmacogenomics is reshaping PK predictions. CPIC 2023 guidelines list 32 gene‑drug pairs where a patient’s CYP genotype changes interaction risk - for instance, CYP2C9*3 carriers are more vulnerable to warfarin‑fluconazole PK clashes.
Artificial intelligence is making headway. A 2023 Nature Medicine paper reported an AI model that predicted PD interactions with 89% accuracy, outpacing traditional rule‑based methods (76%). Hospitals adopting such models see faster alert triage and fewer false positives.
Real‑world evidence continues to surface. FDA’s Sentinel Initiative (2022) identified a 2.3‑fold rise in volume‑depletion risk when SGLT2 inhibitors are paired with loop diuretics - a classic PD interaction that wasn’t on many formularies.
Finally, biologics add a new layer. The EMA’s 2023 Pharmacovigilance report warned that checkpoint inhibitors combined with immunosuppressants can blunt anti‑tumor efficacy, a PD phenomenon that requires careful scheduling.
Quick Checklist for Clinicians
- Ask: Is the interaction PK (dose‑related) or PD (effect‑related)?
- For PK: Identify CYP enzymes or transporters involved; consult the latest Flockhart Table.
- For PD: List overlapping receptor pathways or physiological systems.
- Use TDM for narrow‑index drugs (warfarin, digoxin, phenytoin).
- Consider pharmacogenomic testing when prescribing CYP‑dependent meds.
- Document washout periods for high‑risk PD combos (e.g., MAO‑I ↔ SSRI).
- Leverage EHR alerts but verify clinical relevance - avoid alert fatigue.
- Stay updated on regulatory guidance (FDA, EMA) and emerging AI tools.
Frequently Asked Questions
What is the main difference between PK and PD interactions?
PK interactions alter how much drug reaches the target (the body’s effect on the drug), while PD interactions change what the drug does at the target (the drug’s effect on the body). This distinction guides whether you adjust the dose or avoid the combination.
Which enzymes are responsible for most PK drug interactions?
Cytochrome P450 enzymes, especially CYP3A4, CYP2D6, and CYP2C9, mediate roughly three‑quarters of metabolism‑based interactions.
How can I predict a PD interaction before prescribing?
Map the drugs’ primary targets. If they act on the same receptor (e.g., both are benzodiazepines) or on parallel pathways that converge (e.g., NSAID + ACE inhibitor), a PD interaction is likely. When in doubt, consult a drug‑interaction database or clinical pharmacist.
When is therapeutic drug monitoring essential?
TDM is crucial for drugs with a narrow therapeutic index, such as warfarin (INR), digoxin (serum level), phenytoin (free concentration), and certain antiepileptics. It helps catch PK changes early.
Are there new regulatory requirements for PK/PD studies?
Yes. The FDA’s 2023 draft guidance now expects interaction studies to assess 11 major CYP enzymes and eight transporters, and to include dedicated PD effect assessments when drugs share a therapeutic target.

Kester Strahan
October 24, 2025 AT 14:58When you dive into the ADME matrix, the CYP‑mediated clearance pathways become the linchpin of PK interactions – think of it as the metabolic traffic controller that decides whether a drug gets a green light or a red light.
Antacids chelating quinolones is a classic textbook case; the binding affinity drops the bioavailability by up to 90 % and that’s not a trivial drop, that’s a near‑complete shutdown of systemic exposure.
On the PD side, the synergistic hypotensive cascade between nitrates and sildenafil is a perfect illustration of a pharmacodynamic amplification that bypasses plasma levels altogether.
Clinicians should therefore flag any co‑prescriptions that share the same enzyme or receptor footprint before the patient even steps out of the exam room.
Doreen Collins
October 30, 2025 AT 22:58Mapping the overlapping receptor pathways early can spare patients from dangerous additive effects.
Keep a quick checklist handy: enzyme, transporter, receptor – and you’ll dodge most surprises.
Dawn Bengel
November 6, 2025 AT 10:42Only a fool would ignore the FDA’s CYP guidelines – stupidity hurts patients! 🙄
junior garcia
November 12, 2025 AT 09:02Picture this: two drugs walk into a bar, one blocks the other's receptor and the other says “Not today!” – that’s an antagonistic PD clash in plain English.
When warfarin meets aspirin, the bleed risk spikes dramatically, like fireworks on a calm night.
Remember, if the interaction is PD, adjusting the dose won’t help; you must separate the actors.
Dason Avery
November 18, 2025 AT 06:12The distinction between pharmacokinetic and pharmacodynamic interactions is the cornerstone of modern polypharmacy management.
Pharmacokinetic alterations, driven by enzymes such as CYP3A4, CYP2D6, and transporters like P‑gp, dictate the concentration of a drug that reaches its site of action.
When a strong inhibitor like clarithromycin is introduced, the plasma level of a statin can soar, sometimes tenfold, turning a routine prescription into a potential toxicity nightmare.
Therapeutic drug monitoring becomes the safety net in these scenarios, allowing clinicians to adjust doses based on real‑time serum measurements.
In contrast, pharmacodynamic interactions hinge on the drugs’ mechanisms of effect, independent of their blood levels.
The combination of a beta‑agonist with a beta‑blocker is a textbook antagonistic interaction, where one drug attempts to stimulate the receptor while the other strives to block it, leading to unpredictable cardiac responses.
Synergistic PD effects, such as the infamous pairing of nitrates with sildenafil, can precipitate life‑threatening hypotension, a risk that no amount of dose tweaking can mitigate.
Therefore, the clinical strategy often shifts from dose modification to spatial or temporal separation of the offending agents.
Recent FDA guidance now requires that new drug applications assess interaction potential across an expanded panel of eleven CYP enzymes and eight transporters, widening the safety net for future therapies.
Moreover, the rise of pharmacogenomic testing enables us to personalize risk assessments; a patient carrying the CYP2C9*3 allele, for instance, will metabolize warfarin much more slowly, amplifying any PK interaction with fluconazole.
Artificial intelligence models have also entered the fray, boasting an 89 % accuracy in predicting PD interactions, which can streamline alert triage in crowded electronic health records.
Hospitals that have integrated these AI tools report a noticeable drop in false‑positive alerts, allowing pharmacists to focus on truly high‑risk combos.
Yet, technology is not a panacea; clinicians must still apply clinical judgment, especially when dealing with biologics where immunosuppressants can blunt checkpoint inhibitor efficacy in a PD manner.
In practice, a simple checklist – identify the pathway, verify enzyme or receptor overlap, decide on monitoring or avoidance – can keep the majority of adverse drug events at bay.
Keep this mindset, stay curious, and let the evolving science guide your prescribing habits. 😊
Casey Morris
November 26, 2025 AT 14:45One must appreciate the nuanced interplay of metabolic enzymes, for it is not merely a biochemical footnote but the very fulcrum upon which therapeutic efficacy balances; indeed, overlooking CYP3A4 inhibition in a polypharmacy regimen can precipitate catastrophic toxicity, a fact well‑documented in the annals of clinical pharmacology.
Conversely, the realm of pharmacodynamics demands a sophisticated understanding of receptor pharmacology, as the additive anticoagulant effect of warfarin and aspirin exemplifies the delicate equilibrium of hemostasis.
Thus, the prudent clinician employs therapeutic drug monitoring as a rigorously quantitative adjunct, ensuring that plasma concentrations remain within the narrow therapeutic window.
Moreover, emerging artificial‑intelligence algorithms, while promising, should be scrutinized with the same scholarly rigor applied to traditional interaction studies.
In sum, the confluence of precise measurement, mechanistic insight, and judicious clinical judgment constitutes the hallmark of exemplary patient care.
Teya Arisa
December 2, 2025 AT 09:35Esteemed colleagues, the recent updates to FDA interaction guidelines represent a pivotal advancement in safeguarding patient outcomes.
By mandating evaluation across an expanded spectrum of CYP isoforms and transport proteins, regulatory bodies are fostering a more comprehensive risk assessment framework.
It is incumbent upon prescribers to integrate these recommendations into daily practice, utilizing both therapeutic drug monitoring and, where appropriate, pharmacogenomic testing to personalize therapy.
Such diligent application of evidence‑based principles will undoubtedly mitigate the incidence of adverse drug events.
Thank you for your dedication to continual learning and patient safety. 👍
HILDA GONZALEZ SARAVIA
December 8, 2025 AT 06:52For anyone wrestling with the practical side of interaction checks, a quick tip is to leverage the Flockhart Table alongside your EHR’s built‑in alerts; cross‑reference the listed CYP substrates and inhibitors before finalizing the order.
If you encounter a PD combo such as an SSRI paired with an MAOI, remember the mandatory 14‑day washout period to avert serotonin syndrome.
And don’t forget that many hospitals now embed AI‑driven prediction models, which, while not infallible, can flag obscure PD interactions that static tables might miss.
Bottom line: combine static resources, dynamic alerts, and clinical judgment for the safest prescribing practice.