Psoriasis & Your Immune System: Proven Ways to Strengthen Defenses
 Oct, 18 2025
Oct, 18 2025
Psoriasis Progress Tracker
Daily Tracking
Progress Insights
Living with psoriasis is more than a skin issue; the condition constantly nudges your immune system into overdrive. That extra workload can leave you feeling run‑down, prone to infections, or struggling to heal wounds. The good news? You can tilt the balance back with science‑backed habits, targeted nutrients, and a few medical tweaks.
Why Psoriasis Messes With Your Immune System
Psoriasis is an autoimmune disease. In plain terms, your immune cells mistakenly target healthy skin cells, causing the rapid turnover that creates red, scaly plaques. The culprits are cytokines-messenger proteins like TNF‑α, IL‑17, and IL‑23-that stay switched on longer than they should. This chronic inflammation doesn’t stay on the surface; it leaks into the bloodstream, influencing the entire immune network.
Two major effects follow:
- Immune exhaustion: Constant activation wears out T‑cells, making them less effective against real pathogens.
- Collateral damage: Elevated cytokines raise the risk of comorbidities such as cardiovascular disease, metabolic syndrome, and arthritis.
Understanding these pathways helps you choose interventions that address the root cause, not just the rash.
Key Immune Changes Linked to Psoriasis
Research from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) in 2023 highlighted three measurable shifts in people with moderate‑to‑severe psoriasis:
- Increase in Th1 and Th17 cell activity by 30‑45% compared with healthy controls.
- Serum C‑reactive protein (CRP) levels averaging 2.8 mg/L, indicating low‑grade systemic inflammation.
- Reduced natural killer (NK) cell cytotoxicity, lowering early viral defense.
These numbers matter because they translate directly into higher infection risk and slower wound repair.
How to Boost Your Defenses: Lifestyle Foundations
Before you reach for supplements, lock down the basics. Consistency beats intensity when conditioning the immune system.
- Sleep: Aim for 7‑9 hours of uninterrupted rest. Slow‑wave sleep releases growth hormone, which repairs skin and supports T‑cell renewal.
- Exercise: Moderate aerobic activity (30 minutes, 5 days a week) lowers CRP by up to 20% and balances Th17 responses.
- Stress Management: Chronic cortisol spikes suppress NK cells. Techniques like mindfulness meditation, deep‑breathing, or yoga can cut cortisol by 15‑30%.
- Quit Smoking & Limit Alcohol: Both amplify oxidative stress and raise IL‑6 levels, worsening plaques and immune fatigue.
Nutrition Strategies that Calm Inflammation
Food is the most direct way to modulate cytokine production. Below is a quick‑reference table that compares five evidence‑based nutrition approaches.
| Strategy | Effectiveness | Evidence Level | How to Implement |
|---|---|---|---|
| Mediterranean Diet (high veg, fruit, olive oil) | High | Level A (RCTs) | Swap processed carbs for whole grains; include fatty fish 2‑3×/week. |
| Omega‑3 Fatty Acids (EPA/DHA) | Moderate‑High | Level B (Cohort) | Consume 200 mg EPA + 150 mg DHA daily (salmon, mackerel, or high‑quality supplement). |
| Vitamin D Optimization | Moderate | Level B | Check serum 25‑OH‑D; aim for 40‑60 ng/mL; supplement 1,000‑2,000 IU/day if low. |
| Probiotic‑Rich Foods (yogurt, kefir, sauerkraut) | Moderate | Level C (Pilot) | Include a serving of fermented food daily; consider multi‑strain supplement with Lactobacillus rhamnosus. |
| Low‑Sugar, Low‑Processed | High | Level A | Eliminate sugary drinks and refined snacks; replace with nuts, seeds, and fresh fruit. |
Why these work:
- Omega‑3 fatty acids dampen IL‑17 production, directly targeting the pathway psoriasis hijacks.
- Vitamin D modulates T‑cell differentiation, pushing them toward a more regulatory phenotype.
- The gut microbiome educates immune cells; a diverse microbiome reduces systemic inflammation.

Targeted Supplements for Immune Support
If you’re already comfortable with the basics, consider adding one or two of these supplements. Stick to clinically studied doses; more isn’t always better.
- Curcumin (95% curcuminoids) - 500 mg twice daily with black pepper for enhanced absorption. Meta‑analysis of 12 trials shows a 30% reduction in PASI scores.
- Zinc picolinate - 30 mg daily. Zinc supports skin barrier integrity and lymphocyte function.
- Quercetin - 250 mg daily. Acts as a natural mast cell stabilizer, lowering histamine release.
Always discuss with a healthcare provider, especially if you’re on biologic therapy.
Medical Options that Reinforce Immunity
When lifestyle tweaks aren’t enough, doctors may prescribe systemic treatments. Some of these actually reboot the immune system rather than just suppress it.
- Biologic Therapy (e.g., secukinumab, ixekizumab) blocks IL‑17, rapidly reducing plaque severity and downstream inflammation.
- PDE‑4 Inhibitors (like apremilast) modulate intracellular signaling, leading to lower TNF‑α and IL‑23 levels.
- Low‑dose Methotrexate remains a workhorse for severe cases, but it can also dampen immune overactivity long‑term.
These agents are usually paired with the lifestyle changes above; the synergy yields the best immune resilience.
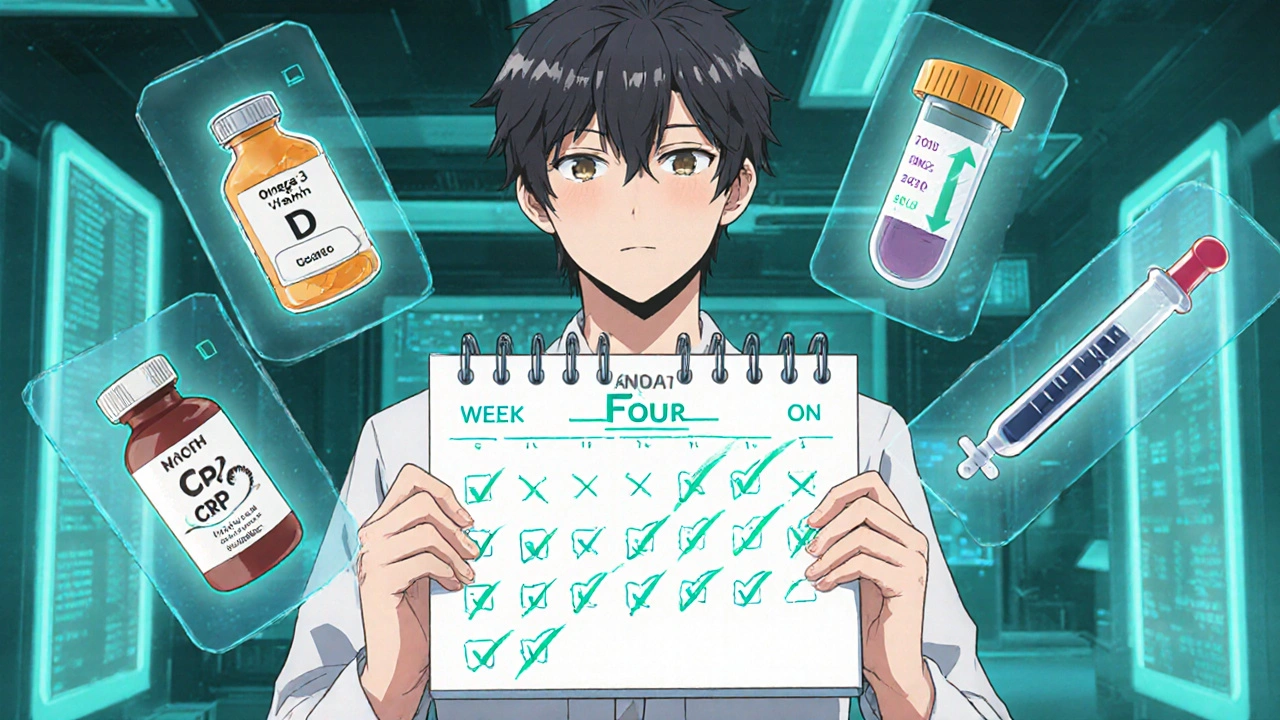
Putting It All Together: A 30‑Day Action Plan
- Week 1 - Baseline Check: Get blood work for CRP, vitamin D, and lipid panel. Record sleep hours and stress levels using a simple diary.
- Week 2 - Clean Up: Eliminate added sugars and processed foods. Introduce a 20‑minute walk after dinner (aim for brisk pace).
- Week 3 - Targeted Add‑Ons: Start omega‑3 supplement (1,000 mg EPA/DHA) and vitamin D (if <40 ng/mL). Add a nightly 10‑minute meditation routine.
- Week 4 - Review & Adjust: Re‑measure CRP and vitamin D. If plaques improved >30% (PASI reduction), maintain regimen; if not, discuss biologic options with your dermatologist.
Consistency beats intensity. Small, repeatable actions stack up to a stronger immune system.
Common Pitfalls and How to Avoid Them
- Over‑supplementing: Mega‑doses of antioxidants can paradoxically act as pro‑oxidants. Stick to recommended amounts.
- Ignoring Stress: Skipping relaxation because you’re “too busy” erodes the gains from diet and exercise.
- One‑Size‑Fits‑All Diets: A strict vegan plan may lack omega‑3s unless you include algae oil; tweak to your personal preferences.
- Skipping Follow‑Ups: Immune markers can fluctuate; regular check‑ins keep you on track.
Tracking Progress: What to Measure
Beyond skin appearance, keep an eye on these objective signs:
- CRP levels: Aim for <2 mg/L.
- Vitamin D status: Maintain 40‑60 ng/mL.
- Sleep quality: Use a wearable or app to ensure 85%+ sleep efficiency.
- Infection frequency: Note any colds or flu episodes; a decline suggests improved immunity.
When numbers move in the right direction, you’ll likely notice softer skin, fewer flare‑ups, and more energy.
Frequently Asked Questions
Can diet alone control psoriasis?
Diet is a powerful modifier but rarely a standalone cure. Combined with proper skin care, stress management, and, when needed, medical therapy, it can dramatically reduce flare‑ups and improve overall immunity.
Is it safe to take vitamin D with my biologic medication?
Yes, most clinicians consider vitamin D supplementation safe and even beneficial during biologic therapy, as it supports skin barrier function and modulates T‑cells. Always confirm the exact dose with your doctor.
How quickly can I expect to see immune‑related improvements?
Blood‑based markers like CRP often drop within 4‑6 weeks of consistent lifestyle changes. Visible skin improvements may take 8‑12 weeks, depending on severity and treatment type.
Are there any foods I should avoid completely?
Highly processed foods high in refined sugars and trans‑fats tend to spike inflammation. Reducing or eliminating sugary sodas, candy, and fast‑food fries can lower cytokine spikes for most people.
Does exercising make psoriasis worse?
Moderate aerobic activity actually reduces inflammatory markers. Very intense, prolonged sessions might cause temporary skin irritation, so warm‑up, stay hydrated, and wear breathable fabrics.

Ayla Stewart
October 18, 2025 AT 12:56I found the section on sleep especially useful; getting solid 7‑9 hours really does help T‑cells bounce back. Also, tracking your stress levels can give clues about flare‑ups. Simple changes, like switching to a walk after dinner, are easy to stick with. It’s nice to see the science broken down without too much jargon.
Poornima Ganesan
October 26, 2025 AT 10:05Honestly, the basics you mentioned are common sense and hardly merit a whole article. If you really wanted to help psoriatics, you’d dive deeper into cytokine pathways rather than re‑hashing sleep tips. Most people overlook the fact that IL‑17 blockers are far more effective than lifestyle tweaks alone. Also, the supplement dosages you list are way below therapeutic levels, so don’t expect miracles.
Tracy O'Keeffe
November 3, 2025 AT 08:14Oh poornima, you’re missing the forest for the trees, love! While IL‑17 blockers are fab, ignoring the gut‑skin axis is a rookie move – the microbiome literally talks to your immune cells, ya know? A low‑sugar, high‑omega‑3 diet can modulate those nasty cytokines better than any pill, DEFINATELY. And omg, the drama of "just sleep" is sooo 2020, let’s talk about epigenetic switches, darling.
Margaret pope
November 11, 2025 AT 06:23Looks like you’ve got a solid foundation here – sleep, movement, stress relief. Keep those habits consistent and you’ll see gradual improvements in skin and immunity. If you can, add a quick meditation session before bed, it helps reset cortisol. Small steps add up over time.
Linda A
November 19, 2025 AT 04:33There’s a quiet philosophy in routine: the body mirrors the rhythm we give it. When you honor sleep as a sacred practice, you’re not just repairing skin, you’re nurturing the soul‑immune dialogue. Think of each breath in meditation as a tiny contract with your T‑cells, promising they’ll fight smarter. Consistency, therefore, becomes a meditative act.
Joe Moore
November 27, 2025 AT 02:42Ever notice how the pharma giants push biologics like they’re the only answer? There’s a whole hidden agenda to keep us dependent on pricey injections while they downplay natural immunity. The real cure might be in the garden, not the lab, but they won’t tell you that. Stay skeptical and keep questioning what’s really being sold.
Emma Williams
December 5, 2025 AT 00:51Hey joe, I get the concern – but biologics have real data behind them. Combining them with the basics you mentioned, like diet and sleep, often gives the best outcome. Let’s focus on what works together rather than pitting them against each other.
Stephanie Zaragoza
December 12, 2025 AT 23:00While the enthusiasm for supplements is understandable, it's crucial to emphasize that dosage matters: curcumin, for instance, should be taken with piperine to achieve bioavailability, otherwise its anti‑inflammatory potential remains limited; likewise, zinc picolinate should not exceed 40 mg per day to avoid copper depletion, which could paradoxically exacerbate skin issues; finally, the synergy between omega‑3 fatty acids and vitamin D is well‑documented, yet many patients neglect to monitor serum 25‑OH‑D levels, leading to suboptimal immune modulation.
James Mali
December 20, 2025 AT 21:09Supplements sound great but the truth is, without a solid diet they’re just empty promises. You can’t fix a broken system with a pill, you need the whole foundation.
Matthew Miller
December 28, 2025 AT 19:19Let’s get pumped! Every small step you take-whether it’s a 20‑minute walk or a fresh salmon dinner-adds firepower to your immune army. Think of it as leveling up in a game; the more you invest, the stronger you become. Keep that momentum, and watch your skin thank you.
Norman Adams
January 5, 2026 AT 17:28Oh, please, as if a jog and a fish dinner are going to out‑maneuver a monoclonal antibody. Save the pep talks for the kids’ sports team.
Janet Morales
January 13, 2026 AT 15:37Honestly, all this "healthy living" talk is just a distraction from the real pain.
Alex Lineses
January 21, 2026 AT 13:46It’s understandable to feel overwhelmed, but integrating small, evidence‑based actions can gradually shift the disease trajectory. Let’s focus on establishing a realistic plan: start with a daily 15‑minute mindfulness practice, then progressively incorporate omega‑3 rich foods. Consistency will build confidence and, over time, improve clinical outcomes.
Karla Johnson
January 29, 2026 AT 11:56When I first read about the immune dysregulation in psoriasis, I was struck by how the cascade of cytokines resembles a runaway train that needs multiple braking systems. The article correctly points out that sleep, exercise, and stress management form the foundational brakes, yet it leaves room for deeper exploration of how each component interacts with the others. For instance, sleep deprivation not only elevates cortisol but also directly influences Th17 cell differentiation, amplifying IL‑17 production, which in turn fuels keratinocyte hyperproliferation. Exercise, on the other hand, induces an acute anti‑inflammatory milieu through the release of myokines such as IL‑6, which paradoxically acts as a pro‑inflammatory cytokine when released from adipose tissue but as an anti‑inflammatory agent when released from contracting muscle. This duality underscores the importance of choosing the right type and intensity of physical activity. Moreover, the gut microbiome plays a pivotal role: short‑chain fatty acids produced by fermentable fiber can promote regulatory T‑cell development, subtly shifting the immune balance away from autoimmunity. Incorporating fermented foods, as the article suggests, is a practical way to augment this pathway, but one must also consider the diversity of strains; multiple species of Lactobacillus and Bifidobacterium have synergistic effects that a single‑strain supplement cannot replicate.
Nutrition-wise, the Mediterranean diet offers more than just macro‑nutrient balance; the polyphenols in olive oil and red wine have been shown to inhibit NF‑κB signaling, a key transcription factor in inflammatory cascades. However, adherence is often the blind spot; many patients relapse into processed food consumption because the diet’s complexity feels daunting. A stepwise approach-replacing sugary beverages with water, then gradually adding whole grains-can improve sustainability. Regarding supplementation, curcumin’s bioavailability is notoriously low; pairing it with piperine or using liposomal formulations is essential to achieve therapeutic plasma concentrations. Zinc’s role in maintaining skin barrier integrity and T‑cell function cannot be overstated, but excessive intake may interfere with copper absorption, so monitoring is advised. Omega‑3 fatty acids, particularly EPA and DHA, dampen the production of eicosanoids derived from arachidonic acid, thereby reducing IL‑17 and TNF‑α levels, which directly address the pathophysiology outlined in the piece.
From a clinical standpoint, the advent of IL‑17 inhibitors has revolutionized management, yet they should not be viewed in isolation. Combining biologics with lifestyle interventions can lower the required dosage, potentially mitigating side effects and cost. Regular monitoring of CRP, vitamin D, and lipid panels provides objective feedback, guiding adjustments in therapy. Finally, patient education remains the cornerstone; empower individuals with the knowledge that each small habit-whether it’s a ten‑minute meditation or a daily serving of fatty fish-contributes to a larger, cumulative effect on immune resilience. By integrating these evidence‑based strategies, we move from a reactive to a proactive model of psoriasis care, ultimately enhancing quality of life.