Remission in Type 2 Diabetes: How Weight Loss and Stopping Medication Can Change Your Health
 Nov, 17 2025
Nov, 17 2025
When you hear "type 2 diabetes," you probably think it’s a lifelong sentence. Pills. Injections. Constant monitoring. But what if that wasn’t the whole story? What if, for some people, the disease could actually go into remission - not just be managed, but quieted down to the point where meds aren’t needed anymore? It’s not magic. It’s science. And it’s happening more often than you think.
What Does "Remission" Really Mean?
Remission in type 2 diabetes isn’t a cure. It doesn’t mean your body suddenly forgot how to struggle with blood sugar. It means your blood sugar has stayed normal for at least three months - without any diabetes meds. That’s the official definition set by the American Diabetes Association, Diabetes UK, the European Association for the Study of Diabetes, and the Endocrine Society in 2021. And it’s not just a suggestion. It’s the standard doctors now use.To qualify, your HbA1c - the test that shows your average blood sugar over the past few months - must be below 48 mmol/mol (6.5%). You can’t get there by taking metformin, GLP-1 drugs, or insulin. Those meds are doing the work, not your body. Remission means your body is doing it on its own. That’s the key.
Some people wonder: "What if my HbA1c is low but I’m still on meds?" That’s not remission. That’s good control. Remission is about freedom from medication. And it’s not just about the number. It’s about what’s happening inside your body - especially your pancreas and liver.
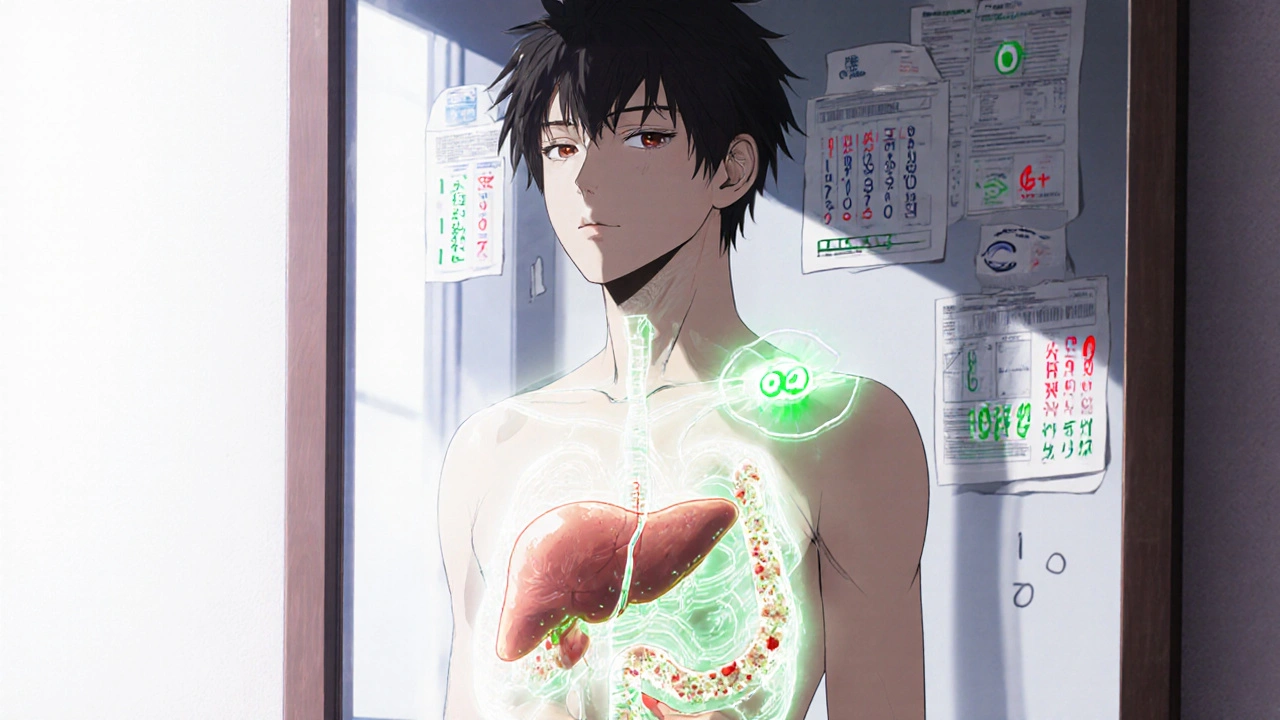
How Weight Loss Makes It Happen
The biggest driver of remission? Losing weight. Not a little. Not "try to eat less." Significant, sustained weight loss. The DiRECT study - one of the most important trials in recent years - showed that 46% of people who lost 10kg or more went into remission after one year. That’s almost half. And the weight loss wasn’t from fancy diets or supplements. It was from a structured, low-calorie plan using meal replacements, followed by gradual food reintroduction and ongoing support.Here’s why it works: When you carry extra fat, especially around your belly, your liver and pancreas get overwhelmed. Fat builds up in the pancreas and blocks insulin production. Your liver starts making too much glucose, even when you don’t need it. Lose that fat, and the organs start working again. The pancreas regains its ability to make insulin. The liver stops flooding your blood with sugar. It’s like rebooting a frozen computer.
The results stick - if you keep the weight off. At two years, remission rates dropped to 36% in the DiRECT study. Why? Because weight came back for some. That’s the catch. Remission isn’t a one-time fix. It’s a long-term commitment to lifestyle.
Who Has the Best Chance?
Not everyone has the same shot at remission. Some people are more likely to succeed - and it’s not about willpower.- Shorter diabetes duration: If you’ve had type 2 for less than five years, your pancreas still has some insulin-making ability left. After that, the cells start dying off. The earlier you act, the better.
- Lower starting HbA1c: If your HbA1c is below 8% when you start, your chances jump. Someone with an HbA1c of 10% or higher has a much harder road.
- No insulin use: People on insulin usually have more advanced disease. Their pancreas has lost too much function. Remission is rare in this group - but not impossible.
- More weight to lose: The more excess weight you carry, the more room there is for improvement. Losing 15kg is more likely to trigger remission than losing 5kg.
That’s why doctors now ask: "How long have you had diabetes?" and "Are you on insulin?" before even talking about remission. It’s not about hoping. It’s about matching the right strategy to the right person.
What About Medication De-escalation?
This is where things get tricky. Some people think stopping meds is dangerous. But when remission is the goal, de-escalation isn’t giving up - it’s testing your body’s new capacity.Doctors don’t just turn off your pills one day. They work with you. They lower the dose slowly. They monitor your blood sugar closely. If your HbA1c stays steady, they keep reducing. If it starts creeping up, they adjust. It’s a careful dance.
And here’s the truth: Not everyone should stop meds just to chase remission. If a drug like semaglutide is helping you lose weight, protecting your heart, and making you feel better - don’t rush to quit it. Dr. Michael Nauck, a leading endocrinologist, says we might need a second category: "remission with medication." Because sometimes, the best way to keep your body healthy is to keep using the tools that help it.
Remission isn’t about being drug-free for pride. It’s about being free from disease burden. If you need a pill to stay healthy, that’s okay. That’s not failure. That’s smart.
What Happens After Remission?
You might think: "I’m in remission. I can eat what I want now." That’s the biggest mistake people make.Even when your HbA1c is normal, the underlying risk doesn’t vanish. Your body still has a tendency toward insulin resistance. Your cardiovascular risk remains higher than someone who never had diabetes. That’s why you still need annual check-ups. You still need to watch your weight. You still need to move.
Studies show that the longer you stay in remission, the lower your risk of complications - nerve damage, kidney problems, eye issues. So even if your blood sugar creeps back up later, you’ve bought yourself years of better health.
The NHS in Scotland puts it plainly: "Remission stops diabetes in its tracks and boosts your chances of a healthy future." But they add: "Blood sugar levels can rise again." That’s why they say: "Keep your appointments. Keep eating well. Keep moving. Even if you feel fine."

The Big Picture: Remission Is Real - But It’s Not Easy
This isn’t a quick fix. It’s not a diet trend. It’s a major life shift. It takes support. It takes time. It takes patience.But the evidence is clear: Type 2 diabetes remission is possible. And it’s not just for the super disciplined. It’s for people who are willing to change - even if they slip up. The DiRECT study included people who had struggled with weight for years. Some gained weight back. But many didn’t. And those who stayed in remission reported better energy, fewer doctor visits, and less anxiety about their health.
What’s holding people back? Often, it’s not lack of knowledge. It’s lack of access. Structured weight loss programs aren’t widely available through the NHS or insurance. Support groups are hard to find. Doctors aren’t always trained to talk about remission as a goal.
But things are changing. The Royal Australian College of General Practitioners added remission guidelines in 2025. The American College of Lifestyle Medicine now has official clinical practice guidelines for it. The conversation is shifting from "manage forever" to "can we reverse?"
What You Can Do Today
If you have type 2 diabetes and want to explore remission:- Ask your doctor: "Is remission a realistic goal for me?" Be ready to talk about how long you’ve had it, your current HbA1c, and whether you’re on insulin.
- Get a baseline HbA1c test. Don’t guess. Know your number.
- Start with weight loss. Aim for 5-10% of your body weight. That’s often enough to see big improvements.
- Look for structured programs. Look for ones that use total diet replacement (like meal shakes) followed by food re-introduction and coaching. These have the strongest evidence.
- Don’t stop meds on your own. Work with your doctor to reduce them safely.
- Keep monitoring. Even if you feel great, get your HbA1c checked yearly.
You don’t need to be perfect. You just need to be consistent. One healthy meal. One walk. One less sugary drink. Those add up.
What’s Still Unknown?
Science doesn’t have all the answers yet. We don’t know exactly how long remission lasts for most people. We don’t know why some relapse and others don’t. We don’t know if remission cuts death risk or just delays complications.Dr. Roy Taylor from Newcastle University says the current definition - three months, HbA1c below 6.5% - is a "working hypothesis." It’s not set in stone. Future studies might change it. Maybe we’ll need longer timeframes. Maybe we’ll find better markers than HbA1c.
But here’s what we do know: Losing weight can change the course of type 2 diabetes. For many, it can mean no pills. No needles. No daily fear. That’s powerful. And it’s worth fighting for.
Can type 2 diabetes be cured?
No, type 2 diabetes cannot be cured. But it can go into remission - meaning blood sugar stays normal for at least three months without medication. The underlying tendency for high blood sugar may still be there, so ongoing lifestyle habits are essential to stay in remission.
How much weight do I need to lose to achieve remission?
Losing 10kg or more significantly increases your chances. In the DiRECT study, people who lost at least 10kg had a 46% remission rate after one year. Even losing 5-7% of your body weight can improve blood sugar control and reduce medication needs.
Do I have to stop all my diabetes meds to be in remission?
Yes. The official definition of remission requires that you’ve been off all glucose-lowering medications for at least three months while maintaining an HbA1c below 6.5%. If you’re still taking metformin, GLP-1 drugs, or insulin, you’re in control - not remission.
Can I eat normally again once I’m in remission?
No. Remission doesn’t mean you can return to your old eating habits. Weight gain is the most common reason remission ends. Staying in remission requires ongoing healthy eating, regular physical activity, and weight maintenance. Think of it as a new way of living, not a temporary fix.
Is remission possible if I’m on insulin?
It’s very rare. People on insulin usually have had diabetes longer and have more damage to their pancreas. While some case reports show remission after major weight loss, it’s not common. Most experts recommend focusing on weight loss and reducing other meds first, but insulin should not be stopped without close medical supervision.
How often should I check my HbA1c after achieving remission?
At least once a year, along with your regular diabetes check-ups. Some doctors may check every six months, especially in the first two years after remission. This helps catch any rise in blood sugar early, before it turns into full-blown diabetes again.

Jenny Lee
November 18, 2025 AT 01:57Remission isn't magic-it's just your body finally getting a break.
Evan Brady
November 19, 2025 AT 10:57People act like remission is some holy grail, but honestly? It’s just biology. Fat in the liver = insulin resistance. Lose the fat = liver wakes up. Pancreas wasn’t dead, just napping. The science’s been clear since 2017. Why are we still acting like this is news? The real tragedy is access-most people can’t afford the DiRECT program, and insurance won’t cover it. That’s not a medical failure. That’s a policy one.
Shravan Jain
November 20, 2025 AT 11:06One must acknowledge the epistemological underpinnings of metabolic remission, wherein the Cartesian dualism of body and mind collapses under the weight (pun intended) of adipose tissue accumulation. The body, as a self-regulating system, exhibits homeostatic plasticity-but only when subjected to sufficient caloric deprivation. The ADA’s definition, while statistically robust, remains reductionist. Remission, in its truest sense, is not a state but a *process*-a continuous negotiation between entropy and order.
Moreover, the notion that insulin users cannot achieve remission is a dangerous oversimplification. Insulin resistance is not synonymous with beta-cell death. I have reviewed case studies from Bangalore where patients on long-term basal insulin achieved HbA1c <6.0% after bariatric surgery and sustained lifestyle intervention. The paradigm is shifting. We must stop conflating duration with irreversibility.
And yet, the pharmaceutical-industrial complex thrives on the myth of chronicity. Metformin is cheap. GLP-1 agonists? Not so much. Who benefits from the narrative that diabetes is a life sentence? The answer is written in quarterly earnings reports.
Remission is not about willpower. It is about structural access. A man in rural Rajasthan cannot replicate the DiRECT protocol. He has no meal replacements. No dietitian. No Wi-Fi to watch YouTube tutorials. To tell him he’s failed because he didn’t lose 10kg is not science. It is colonialism in lab coats.
The HbA1c metric itself is flawed. It averages. It ignores spikes. It ignores glycemic variability. A person could have a 6.4% HbA1c and still be in constant hyperglycemic distress. Or they could have a 6.6% and be metabolically stable. We need dynamic biomarkers. Continuous glucose monitoring should be standard. Not optional.
And yet, here we are, debating whether someone who lost 12kg and stopped metformin is ‘in remission’-while the real crisis is that 80% of diabetics in low-income countries don’t even have access to test strips.
Remission is a privilege. And we are treating it like a moral victory.
Let us not celebrate the few who escaped the cage while ignoring the millions still locked inside.
But I suppose, in a world where healthcare is a market, the only thing that matters is the number on the screen. Not the life behind it.
Brandon Lowi
November 21, 2025 AT 05:36America’s got the best science, the best doctors, the best diets-and still, we let Big Pharma convince folks that diabetes is a life sentence? That’s not science, that’s surrender. We’ve got the tools to flip the script, but instead, we’re outsourcing our health to pills made in China and India while our own system chokes on bureaucracy. If you’re on insulin and still think you’re ‘in control,’ you’re not controlling anything-you’re being controlled. Remission isn’t a perk. It’s your birthright. Stop letting corporations dictate your biology.
And don’t even get me started on how the NHS and WHO are still dragging their feet. We’re talking about reversing a disease that costs the U.S. $400 billion a year. You think they care? Nah. They care about stock prices. I’ve seen it. I’ve lived it.
Richard Couron
November 21, 2025 AT 12:39They’re hiding something. Why does everyone act like weight loss is the only path? What about glyphosate? What about the fluoridated water? The CDC won’t admit it, but diabetes is a bioweapon experiment gone wrong-designed to keep people docile, dependent on meds, and too tired to protest. You think it’s coincidence that as Big Pharma profits soared, diabetes rates exploded? Wake up. The ‘remission’ narrative is just a distraction. They want you to think you’re in control… while they control your insulin supply chain. The real cure? Get off the grid. Eat real food. Stop trusting ‘experts.’
Alex Boozan
November 22, 2025 AT 02:39From a clinical endocrinology standpoint, the concept of remission is fundamentally misaligned with the pathophysiology of T2DM. Beta-cell dysfunction is progressive. Even in cases of apparent HbA1c normalization, residual beta-cell exhaustion persists. The DiRECT study’s 46% remission rate is statistically significant but clinically misleading-because it ignores the heterogeneity of adipose tissue distribution. Visceral adiposity is the real driver, not BMI. And the study’s cohort was highly selected: younger, non-insulin-dependent, with shorter disease duration. Generalizing this to the broader population is a category error.
Moreover, the term ‘remission’ implies temporary resolution, which is accurate-but the medical community has failed to communicate the lifelong vigilance required. Patients interpret ‘remission’ as ‘cured’ and revert to pre-diagnostic behaviors. The relapse rate is not a failure of the patient-it’s a failure of counseling.
Also, why is there no mention of circadian rhythm disruption? Sleep apnea? Gut microbiome dysbiosis? These are co-conspirators in metabolic collapse. Fixing weight alone is like mopping the floor while the faucet is still on.
mithun mohanta
November 22, 2025 AT 02:43Oh wow, another ‘you can reverse diabetes if you just lose weight’ lecture-how original. I’ve seen this same article 12 times on Medium. People act like it’s revolutionary, but in India, we’ve known this since the 80s. Our grandparents didn’t have diabetes because they didn’t eat ‘meal replacements’-they ate dal, roti, and walked 10km a day. Now we’re all sipping protein shakes and calling it ‘health.’ Pathetic. Also, why is everyone obsessed with HbA1c? My uncle’s was 6.2% and he still had a stroke. Numbers lie. Your body doesn’t.
And let’s be real-no one’s gonna lose 10kg unless they’re already rich enough to afford gyms and organic kale. This isn’t science. It’s capitalism with a stethoscope.
Ram tech
November 24, 2025 AT 00:24Remission? Yeah right. You think losing weight fixes anything? My cousin lost 30lbs, stopped meds, felt great for 6 months… then went back to eating biryani and now his HbA1c’s 9.8. He’s worse off. This whole thing is a scam to sell diet plans. People don’t change. They just get bored and give up. Don’t believe the hype.
Jeff Hakojarvi
November 24, 2025 AT 03:19I’ve helped dozens of patients through remission, and the biggest thing I’ve learned? It’s not about the number on the scale-it’s about the number of people who show up for you. The ones who cook with you. Who walk with you. Who don’t judge when you slip. Remission doesn’t happen in isolation. It happens in community. If you’re trying to do this alone, you’re already fighting an uphill battle. Find your people. Even if it’s just one friend who texts you every morning: ‘Did you drink water today?’ That’s the real medicine.
And if you’re on insulin? Don’t panic. Some of my best remission stories started with insulin. We tapered slowly. We focused on sleep, stress, movement-not just calories. It’s not magic. It’s patience. And you’re not failing if it takes time. You’re learning.
Timothy Uchechukwu
November 25, 2025 AT 22:15Why do Westerners think they invented health? In Nigeria we’ve always known that food is medicine. Our ancestors didn’t need meal replacements. They ate yam, plantain, bitter leaf soup. Now we’re drinking protein shakes and calling it progress? This is cultural erasure dressed as science. The real issue is not fat-it’s the colonial mindset that tells us our way of eating is inferior. Remission? We never lost it in the first place.
Ancel Fortuin
November 27, 2025 AT 09:33Oh sure, let’s all celebrate remission like it’s some miracle. Meanwhile, the same people who wrote this article are probably sipping oat milk lattes in Palo Alto while the rest of us are choosing between insulin and rent. You call this science? It’s a luxury. And if you think losing weight is the answer, you’ve never had to work three jobs, sleep 4 hours, and eat whatever’s cheapest. Remission is for people who can afford to care.
Also, ‘no meds’? Funny. My cousin got kicked off Medicaid last year. He stopped his meds not because he was in remission-he stopped because he couldn’t afford them. His HbA1c’s now 11.2. Is he in remission? Or just broke?
Hannah Blower
November 28, 2025 AT 05:17Let’s be brutally honest: remission is just the pharmaceutical industry’s way of selling you a new product-‘The Life You’ll Live After You Stop Taking Our Drugs.’ The entire narrative is engineered to make you feel guilty if you don’t achieve it. You’re not lazy if you can’t lose weight. You’re not weak if you need insulin. You’re just a human being in a broken system that profits from your suffering. The real cure? Universal healthcare. Not a 1200-calorie shake.
Gregory Gonzalez
November 29, 2025 AT 12:45How quaint. The idea that diabetes can be ‘reversed’ by diet alone, as if we’re all just one Whole30 away from enlightenment. The truth? Most people who ‘achieve remission’ are young, white, wealthy, and had diabetes for less than two years. The rest? They’re told to ‘try harder.’ And when they fail? They’re labeled ‘non-compliant.’ This isn’t medicine. It’s moralizing with a stethoscope.
And the fact that we’re still using HbA1c as the gold standard? Please. It’s like judging a symphony by how loud one violin plays.
Evan Brady
December 1, 2025 AT 10:35Jeff, you nailed it. Community is everything. I’ve seen people relapse not because they wanted to, but because they lost their support group. Job change. Move. Death of a friend. No one to walk with. No one to cook with. It’s not about willpower. It’s about belonging. We need to build systems that keep people connected-not just tell them to ‘eat better.’