Shared Decision-Making in Autoimmune Care: Balancing Risks and Benefits
 Feb, 3 2026
Feb, 3 2026
When you’re living with an autoimmune disease like rheumatoid arthritis, multiple sclerosis, or lupus, every treatment choice comes with trade-offs. One drug might cut your flare-ups in half-but it could also raise your risk of a rare, life-threatening infection. Another might be easier to take but less effective. In these situations, the best decision isn’t just about the science. It’s about your life. That’s where shared decision-making comes in.
What Shared Decision-Making Really Means
Shared decision-making (SDM) isn’t just a buzzword. It’s a structured way for you and your doctor to work together to pick the right treatment. Gone are the days when doctors simply told you what to do. Today, SDM means you’re not just a passive recipient of care-you’re an active partner. The process starts with honest conversation. Your doctor doesn’t just hand you a pamphlet and say, "Take this." Instead, they ask: "What matters most to you?" Do you need to travel often? Are you planning a pregnancy? Are you terrified of needles? These aren’t small details-they’re deal-breakers. Studies show that when patients are truly involved, they stick with their treatment longer. In one study of over 3,000 people with autoimmune conditions, 82% stayed on their prescribed therapy when they’d made the choice alongside their doctor. That’s compared to just 63% when decisions were made without them.How It Works: The Three Talking Phases
Real shared decision-making follows a clear structure, usually taking just 9 to 14 minutes in a typical appointment. It breaks down into three simple steps:- Team Talk - "We’re in this together." Your doctor checks in: "What do you already know? What are you worried about?" This builds trust before diving into options.
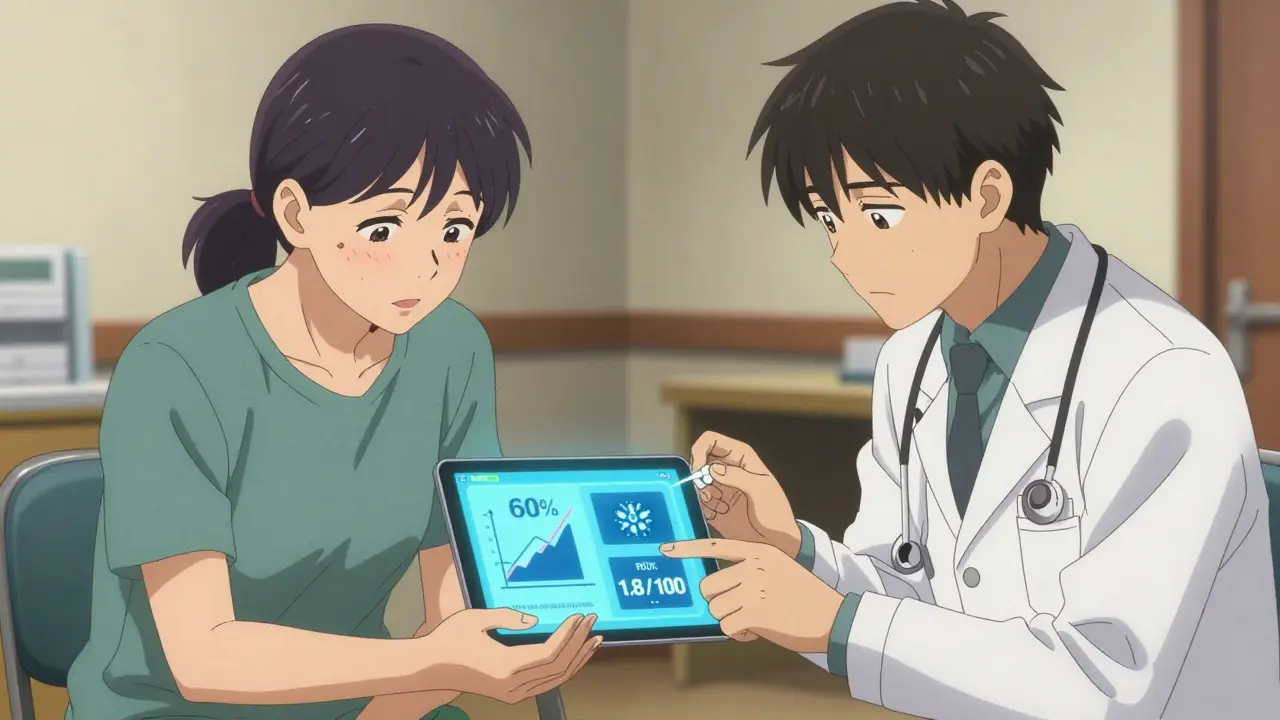
- Option Talk - "Here’s what’s possible." No vague promises. Instead, clear numbers: "This drug reduces flares by 60%, but 1.8 out of every 100 people get a serious infection each year." Tools like decision aids-videos, booklets, or apps-show these risks visually, not just as percentages.
- Decision Talk - "What feels right for you?" You weigh the numbers against your life. Maybe you choose the less effective pill because you can’t handle monthly infusions. That’s okay. And your doctor should be okay with it too.
One patient, a nurse with rheumatoid arthritis, told her rheumatologist she couldn’t miss work for weekly injections. Together, they switched from an injectable biologic to an oral drug. Her disease stayed controlled. Her job didn’t suffer. That’s SDM in action.
Why It Matters More in Autoimmune Diseases
Autoimmune conditions are tricky because they don’t follow a one-size-fits-all path. Two people with the same diagnosis can have wildly different experiences. One might have mild joint pain. Another might face organ damage. Treatment options vary just as much. Take multiple sclerosis. Some drugs can reduce relapses by 70%. But one of them, natalizumab, carries a 1 in 1,000 risk of a rare brain infection called PML. If you’re young, active, and planning a family, you might say: "I’ll take the risk." If you’re older, with other health issues, you might say: "No thanks." Your doctor can’t make that call for you. Same goes for rheumatoid arthritis. Methotrexate is cheap and effective for many. But if you’re trying to get pregnant, your doctor won’t even consider it. Biologics like adalimumab work better for some-but they raise infection risk. A 2021 study found patients who used decision aids were 41% more likely to understand their options. And those who understood? They were far less likely to quit treatment later.What’s Missing in Most Clinics
Here’s the problem: most doctors want to do SDM. But they don’t have the time, tools, or training. A 2021 survey of rheumatologists found that 78% said they’d love to use decision aids-but they never get around to it. Appointments are 15 minutes long. Insurance doesn’t pay extra for the extra time it takes to explain risks properly. And many providers still rely on outdated habits: "This is the best option," or "I’ve seen this work for others." Worse, some patients leave appointments confused. One woman with MS said her neurologist listed three drugs in 90 seconds. No discussion. No visuals. Just names. She picked one blindly-and stopped taking it six months later because it made her too tired to care for her kids. The gap isn’t about intent. It’s about systems. Only 22% of rheumatologists consistently use validated decision aids, even though 89% say they believe in them.Tools That Actually Help
The good news? Tools exist-and they work. The Arthritis Foundation offers free, easy-to-use decision aids for RA, psoriatic arthritis, and lupus. They’re used by over 150,000 people since 2017. The National MS Society’s "MS Values" tool asks you to rank what matters most: preventing relapses? Avoiding hospital visits? Staying active? Then it matches you with drugs that fit. The University of Michigan’s "MS Decisions" tool changed how risks are shown. Instead of saying "0.1% risk of PML," it says: "1 in 1,000 chance over two years." That’s clearer. And patients love it. One review called it "the only thing that made me feel like I wasn’t being sold a cure." Even AI is stepping in. In March 2023, the FDA cleared the first AI-powered tool for rheumatoid arthritis called ArthritisIQ. It pulls data from your EHR, your symptoms, and your lifestyle to generate a personalized risk-benefit report. It doesn’t decide for you. It just makes the choices easier to understand.
When Shared Decision-Making Doesn’t Work
SDM isn’t magic. It doesn’t work in emergencies. If you’re having a severe flare-swollen joints, high fever, sudden vision loss-you need treatment now. There’s no time for a 10-minute chat. A 2020 study found nearly half of rheumatologists said SDM was impossible during acute flares. That’s fine. But here’s the catch: even in those moments, you should still be asked: "What would you want if this keeps happening?" That way, when things calm down, you’re not starting from scratch. Another problem? Health literacy. If you don’t understand numbers, statistics, or medical terms, you can’t make informed choices. That’s why visual aids matter. A graph showing "1 in 100" is better than "1%". A picture of a needle versus a pill? That speaks louder than a paragraph. And then there’s the digital divide. Older patients, those with lower education, or people without smartphones get left behind. One study found they get 37% less benefit from digital tools without extra help-like a nurse sitting with them, walking through the app.What You Can Do
You don’t have to wait for your doctor to lead. You can start this conversation yourself. Before your next appointment:- Write down your top three concerns: pain? fatigue? side effects? travel?
- Ask: "What are my options?" and "What are the real risks?"
- Request a decision aid. Many are free online.
- Ask: "Can we go over the numbers? I want to understand what "1 in 1,000" really means."
And if your doctor brushes you off? Push back. You have the right to understand your care. You’re not asking for special treatment-you’re asking for standard care.
The Bigger Picture
This isn’t just about one appointment. It’s about a system that’s changing. Medicare now ties 9% of payments to patient experience scores-scores that include whether you felt involved in decisions. The European League Against Rheumatism requires SDM documentation for biologic prescriptions. And the U.S. government now mandates decision aids for certain treatments under the 21st Century Cures Act. The message is clear: shared decision-making isn’t optional anymore. It’s part of the standard of care. And for people with autoimmune diseases? It’s the difference between managing a condition-and truly living with it.What is shared decision-making in autoimmune care?
Shared decision-making (SDM) is a collaborative process where patients and healthcare providers work together to choose the best treatment based on both clinical evidence and the patient’s personal values, lifestyle, and preferences. It’s especially important in autoimmune diseases because treatments often involve serious trade-offs between effectiveness and side effects.
Why is shared decision-making better than the old "doctor knows best" model?
The old model often led to low adherence because patients didn’t understand or agree with the treatment. SDM improves outcomes by aligning choices with what matters most to the patient. Studies show 82% of patients stick with their treatment when they’ve helped choose it, compared to just 63% when decisions are made without them.
What tools are available to help with shared decision-making?
Free, evidence-based decision aids are available from organizations like the Arthritis Foundation and the National MS Society. These include interactive tools, videos, and booklets that show exact risks and benefits-for example, "60% of patients see improvement with this drug, but 1.8 out of 100 get serious infections each year." AI-powered tools like ArthritisIQ now also generate personalized risk profiles based on your health data.
Can shared decision-making be used during a disease flare?
During an acute flare, immediate treatment is often needed, and there isn’t time for lengthy discussions. However, even in emergencies, it’s valuable to ask: "What would you prefer if this keeps happening?" That way, once the crisis passes, you’re already aligned on long-term goals.
How can I prepare for a shared decision-making conversation with my doctor?
Before your appointment, write down: 1) Your biggest concerns (pain, fatigue, side effects), 2) Your lifestyle needs (travel, work, family), and 3) Questions like: "What are my options?" and "What are the real risks?" Bring up decision aids if your doctor hasn’t offered them. You have the right to understand your care fully.
Do insurance plans cover shared decision-making tools?
Most decision aids are free and not billed to insurance. However, some insurance systems, including Medicare Advantage, now tie payments to patient experience scores that include shared decision-making. The 21st Century Cures Act also requires decision aids for certain Medicare-covered treatments, including autoimmune biologics.
Is shared decision-making only for people with rheumatoid arthritis or MS?
No. SDM applies to all autoimmune conditions-including lupus, psoriatic arthritis, Crohn’s disease, and others-where treatment choices involve balancing effectiveness with serious side effects. The same principles apply: clear risks, personal values, and joint decision-making.

Katharine Meiler
February 4, 2026 AT 06:32Shared decision-making isn’t just a nice-to-have-it’s the backbone of sustainable care in autoimmune conditions. The data’s clear: 82% adherence when patients co-decide versus 63% when they don’t. That’s not anecdotal. That’s statistically significant. And it’s not just about compliance-it’s about agency. When you’re the one choosing between monthly infusions and oral meds, you’re not a patient. You’re a stakeholder. The real win? When your doctor stops saying "this is standard" and starts asking "what’s tolerable for you?" That shift-from paternalism to partnership-is what finally makes treatment stick.
Decision aids aren’t fluff. They’re translation tools. Turning "1.8 per 100" into a visual risk matrix? That’s not dumbing down. That’s equity. People don’t need to be doctors. They need to understand trade-offs in their language. And yeah, AI tools like ArthritisIQ? Finally. Something that pulls from EHRs, lifestyle, and symptom logs to generate a personalized risk profile. No more guessing. Just data, framed for human context.
Danielle Vila
February 5, 2026 AT 14:03Okay but have you ever heard of the BIG PHARMA shadow network? They don’t want you making decisions-they want you dependent. These "decision aids"? Paid for by drug companies. The 82% adherence stat? Sponsored by biologics manufacturers. And don’t get me started on ArthritisIQ-FDA-cleared? Please. That’s just a fancy algorithm trained on data that excludes elderly, low-income, and non-English-speaking patients. They’re not helping you-they’re conditioning you to trust the system that’s been poisoning you with side effects for decades. I’ve seen it. My cousin took adalimumab. Lost her spleen. Now she’s on six meds. "Shared decision-making"? More like shared exploitation. They want you to think you’re in control… while they’re just swapping one pill for another with a prettier label.
Thorben Westerhuys
February 7, 2026 AT 10:42I just… I need to say this. I’ve been living with lupus for 12 years. I’ve had three flares that put me in the hospital. I’ve cried in parking lots after appointments because I felt like a burden. And then-finally-my rheumatologist sat down with me. Not in a rush. Not with a pamphlet. She said: "Tell me what you’re scared of." And I said: "I can’t handle needles. I can’t miss work. I can’t be tired all the time." And she didn’t push. She didn’t lecture. She showed me a chart. A real one. With pictures. And we picked an oral drug. Not the "best" one. Not the newest. The one that let me hug my daughter without shaking.
I’m not saying this for praise. I’m saying it because I need someone else to know: it’s possible. You don’t have to be a hero to get good care. You just have to be heard. And if your doctor won’t listen? Find someone who will. You deserve that. I didn’t think I did. I was wrong.
Laissa Peixoto
February 9, 2026 AT 07:10There’s a deeper philosophical layer here that’s being overlooked. Shared decision-making isn’t just a clinical protocol-it’s an epistemological shift. It challenges the Cartesian model of the physician as omniscient agent and the patient as passive vessel. Instead, it proposes a phenomenological co-construction of meaning: the patient’s lived experience becomes not just data, but a valid epistemic source alongside biomarkers and clinical trials.
This is radical. It requires redefining expertise. Not as "knowledge possessed," but as "knowledge co-created." The numbers matter-but so does the weight of a child’s cry at 3 a.m. The 1.8% infection risk is statistically real-but so is the terror of losing your job, your independence, your identity. The real innovation isn’t in the tools. It’s in the humility of the clinician who says: "I don’t know what’s right for you. But I’ll help you find out."
And yet… we still measure success in adherence rates, not in quality of life metrics. We’re still stuck in a biomedical paradigm that reduces personhood to risk factors. Until we center the narrative-not the numbers-we’re just automating alienation with better UIs.
Lana Younis
February 9, 2026 AT 12:42Y’all are overcomplicating this. Look-I’ve got RA. I’m a single mom. I work retail. I don’t have time to read 10-page decision aids. But I do have my phone. And I do have 5 minutes between shifts.
The Arthritis Foundation app? Saved me. It had a slider: "How much do you care about avoiding hospital visits vs. stopping pain?" I slid it all the way to "avoid hospital visits." It said: "Try this oral med. Less risky. Slower results." I tried it. Worked. No infusions. No missed work.
And yeah, I misspelled "medication" in the chat. Whatever. The point is: if it’s not accessible, it’s not helpful. Tools gotta be dumb-simple. Visual. Mobile. No jargon. No 14-minute consults. Just: here’s your option. Here’s the trade. You decide.
Also-doctors? Stop saying "1 in 100." Say "one person out of every classroom of kids." That’s what sticks.
Samantha Beye
February 9, 2026 AT 14:36I’m not a doctor. I’m a caregiver. My mom has MS. She used to say "I just want to live." Not "I want to be cured." Not "I want the best drug." Just… live.
When we finally sat down with her neurologist and used the MS Values tool? It was the first time she smiled during a consult. She picked "staying active with my grandkids" as her top priority. The tool showed her that one drug had higher relapse prevention-but 37% of users reported extreme fatigue. She chose the other one. Not because it was "weaker." Because it let her push her grandson on the swing.
That’s not medicine. That’s love. And it’s not rare. It’s just… rarely asked for. Ask your doctor: "What does living well look like for me?" Not what’s optimal. What’s possible. And then-listen. Really listen. That’s the real decision-making.
Rene Krikhaar
February 11, 2026 AT 11:31Lisa Scott
February 11, 2026 AT 20:05Let’s cut the BS. SDM is a marketing ploy wrapped in placebo science. The 82% adherence stat? Cherry-picked from trials where patients were incentivized. The decision aids? Designed to nudge you toward expensive biologics. And the FDA clearance of ArthritisIQ? That’s regulatory capture. They don’t want you to understand-they want you to trust. The real risk isn’t infection. It’s compliance. You think you’re choosing? You’re being guided toward the most profitable option. Your doctor gets paid more when you start a biologic. The system isn’t broken. It’s working exactly as designed. And you? You’re the revenue stream.
Dina Santorelli
February 13, 2026 AT 19:22I’m not even mad. I’m just… tired. I’ve been through three rheumatologists. Each one said "we’ll find the right fit." None of them asked what fit meant to me. One told me to "just be grateful" I wasn’t on chemo. Another said "you’re lucky you’re young enough for this."
I stopped going to appointments. I read the papers myself. Found the decision aids. Made my choice. Took the oral drug. No infusions. No ER visits. Just… me. And my cat. And my quiet life.
They say SDM is about partnership. But I didn’t find a partner. I found a loophole. And I’m not sorry.
Katharine Meiler
February 15, 2026 AT 07:30Replying to @7480: You’re right to be skeptical. The system is rigged. But throwing out SDM because of corruption is like refusing to eat because the kitchen is messy. The tools still work-even if the incentives are broken. I’ve seen patients use decision aids to say NO to expensive biologics. To choose methotrexate over Humira. To refuse a drug because the infection risk didn’t match their values. SDM doesn’t fix Big Pharma. But it gives patients a lever. And sometimes? That’s enough to crack the door open.