Topical Medication Allergies: How to Spot and Treat Contact Dermatitis
 Dec, 25 2025
Dec, 25 2025
What Is Topical Medication Allergy?
You put on a cream for your rash, and instead of getting better, your skin gets worse. It burns, itches, turns red, and spreads. You think it’s getting infected. Maybe you doubled the dose. But what if the medicine itself is the problem? That’s topical medication allergy - a hidden reaction many doctors miss because they assume the treatment can’t cause the problem.
This isn’t just a mild irritation. It’s allergic contact dermatitis: a delayed immune response to something in your lotion, ointment, or gel. It doesn’t show up right away. It takes 24 to 72 hours after contact. And it’s more common than you think. About 1 in 6 people who get patch tested for stubborn rashes turn out to be allergic to a topical medication - not poison ivy, not perfume, but something prescribed to help them.
Why Your ‘Treatment’ Is Making Things Worse
Think about this: if you’re using hydrocortisone cream for eczema, and your skin flares up after a week, you might blame stress, soap, or dry air. But what if the hydrocortisone is the trigger? That’s not rare. About 0.5% to 2.2% of people using topical steroids develop an allergy to them. In other words, the very drug meant to calm your skin is lighting it on fire.
Antibiotics are even bigger culprits. Neomycin - found in over-the-counter first aid creams like Neosporin - shows up in nearly 1 in 10 positive patch tests. Bacitracin and gentamicin aren’t far behind. Local anesthetics like benzocaine (in numbing sprays and gels) and NSAIDs like ketoprofen (in pain-relief gels) are also common triggers. And here’s the twist: many of these aren’t even prescription drugs. They’re in the stuff you grab off the pharmacy shelf without thinking.
Even corticosteroids themselves can cause cross-reactions. If you’re allergic to hydrocortisone (Group A steroid), you might safely use triamcinolone (Group B) or methylprednisolone (Group D). But if you don’t know the group, you could keep switching creams and making it worse.
How to Tell It’s Allergic - Not Just Irritated
Not every red, itchy patch is an allergy. Most skin reactions from topical products are irritant contact dermatitis - a simple burn from harsh chemicals, not an immune response. The difference matters because treatment changes completely.
Here’s how to tell:
- Allergic contact dermatitis: Itchy, red, sometimes blistering rash that spreads beyond where you applied the product. It shows up 1-3 days later. Often looks like a pattern - like the shape of the bandage or the area you rubbed the cream on.
- Irritant contact dermatitis: Burning or stinging right after application. Rash stays where you applied it. No spreading. More common in people with dry, cracked skin or who wash their hands too much.
Studies show 15% to 20% of people who think they’re allergic to topical meds are actually just irritated. That’s why patch testing isn’t optional - it’s essential.
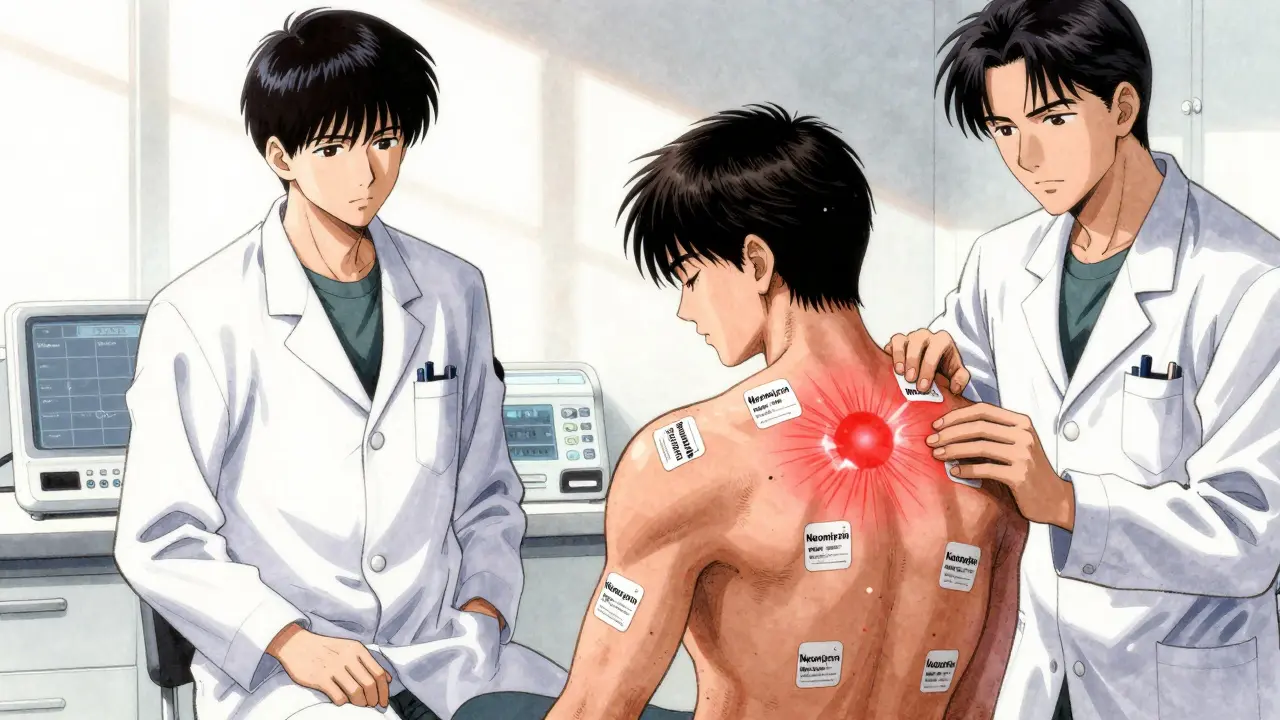
What Is Patch Testing, and How Does It Work?
Patch testing is the gold standard for diagnosing allergic contact dermatitis. It’s not a skin prick. It’s not a blood test. It’s a slow, quiet process that reveals what your skin is quietly screaming about.
Here’s how it works:
- You visit a dermatologist or allergist who specializes in contact allergies.
- Small patches with suspected allergens - including common medications like neomycin, corticosteroids, lidocaine, and ketoprofen - are taped to your back.
- You leave them on for 48 hours. No showering, no sweating, no removing them.
- At 48 and 96 hours, the patches come off and your skin is checked for reactions.
It’s not perfect - about 70% of cases get confirmed this way - but it’s the best tool we have. And here’s the kicker: in 2023, Johns Hopkins researchers found that diluting the medication 10 times before patch testing cuts false negatives by more than half. That’s huge for people with broken skin barriers who used to get negative results even when they were allergic.
And yes - you should bring every product you use on your skin to the appointment. That includes your shampoo, moisturizer, sunscreen, and even your partner’s lotion. Thirty percent of triggers are found in non-medication products you never thought of as risky.
How to Treat It - Without Making It Worse
Once you know what you’re allergic to, the most important step is simple: stop using it. No exceptions. Even small amounts can keep the reaction going.
For mild cases, over-the-counter 1% hydrocortisone cream can help - but only if you’re not allergic to it. If you are, skip it. Instead, try:
- Calcineurin inhibitors: Pimecrolimus (Elidel) or tacrolimus (Protopic). These aren’t steroids. They’re immunomodulators. Studies show 60-70% of patients see improvement within 2 weeks. Side effect? A temporary burning feeling for the first few days - but no skin thinning.
- Low-potency steroids: Desonide 0.05% ointment for sensitive areas like eyelids, face, or groin. Avoid high-potency steroids like clobetasol here - they can cause skin atrophy in up to 35% of users after two weeks.
- Systemic steroids: If more than 20% of your skin is affected, you’ll need oral prednisone. Doses of 40-60 mg daily usually bring relief in under 24 hours. But taper slowly - stopping too fast can cause rebound flares.
And here’s something most people don’t know: the American Academy of Dermatology found that 89% of chronic cases resolve within 4 weeks - only if the allergen is removed. With just medication and no avoidance, only 32% get better.

What to Avoid - and What to Use Instead
Once you’re diagnosed, you need a new skincare routine. Here’s what to ditch:
- Products with neomycin, bacitracin, or benzocaine - even if they’re labeled ‘natural’ or ‘gentle’.
- Medicated wipes, numbing sprays, or anti-itch creams with unknown ingredients.
- Generic store-brand ointments - they often contain hidden allergens.
Instead, look for:
- Simple, fragrance-free moisturizers with minimal ingredients - like CeraVe or Vanicream.
- Products labeled ‘hypoallergenic’ and ‘patch-tested’ - but verify the ingredients yourself.
- Barrier creams with ceramides or squalane - they help rebuild your skin’s natural defense.
And use the American Contact Dermatitis Society’s free mobile app. It lets you scan product barcodes and check for 3,500+ allergens. Over 40% of patch-tested patients use it to avoid hidden triggers.
Why This Is Still Overlooked - And What’s Changing
Dr. Erin Warshaw, former president of the American Contact Dermatitis Society, says it plainly: ‘Clinicians assume the treatment can’t be the cause.’ That’s why 40-60% of cases are misdiagnosed at first.
Patients report spending 6+ months and visiting 3+ doctors before getting the right diagnosis. On Reddit, one person wrote: ‘I used steroid cream for 18 months thinking it was my eczema. It was the steroid.’
But things are shifting. The FDA now requires full ingredient lists on all topical prescriptions. Patch testing use has jumped 27% since 2018. And in 2023, researchers introduced a new ‘Topical Medication Allergy Score’ that improves diagnosis accuracy from 65% to 89%.
Even bigger: the NIH just funded $4.7 million to develop a test that could predict your allergy risk before you even use a cream. Imagine avoiding this whole problem before it starts.
What to Do Next
If your skin isn’t improving - or is getting worse - after using a topical product:
- Stop using everything new you’ve added in the last 2 weeks.
- Switch to a plain, fragrance-free moisturizer (CeraVe or Vanicream).
- Take a photo of your rash and write down every product you’ve used on that area - including toothpaste or shampoo if it touched your neck or face.
- Ask your doctor for a referral to a dermatologist who does patch testing.
- Don’t accept ‘it’s just eczema’ if the treatment isn’t working.
Topical medication allergies are treatable. But only if you know what you’re allergic to. And that starts with asking the right question: ‘Could this cream be making me worse?’

jesse chen
December 26, 2025 AT 03:13Joanne Smith
December 27, 2025 AT 09:48Prasanthi Kontemukkala
December 28, 2025 AT 18:20Bryan Woods
December 29, 2025 AT 11:41Ryan Cheng
December 30, 2025 AT 05:11Shreyash Gupta
December 31, 2025 AT 23:13Ellie Stretshberry
January 2, 2026 AT 02:17Angela Spagnolo
January 2, 2026 AT 09:50Sarah Holmes
January 2, 2026 AT 14:30Jay Ara
January 4, 2026 AT 13:10Michael Bond
January 5, 2026 AT 12:49SHAKTI BHARDWAJ
January 5, 2026 AT 16:18