Diabetes Remission Criteria: What It Really Means and How It Works
When we talk about diabetes remission criteria, the specific medical benchmarks used to determine if type 2 diabetes has reversed without ongoing medication. Also known as diabetes reversal, it’s not a cure—but it’s close enough to change how people live. This isn’t wishful thinking. It’s backed by real data from clinical studies, and it’s happening more often than you might think.
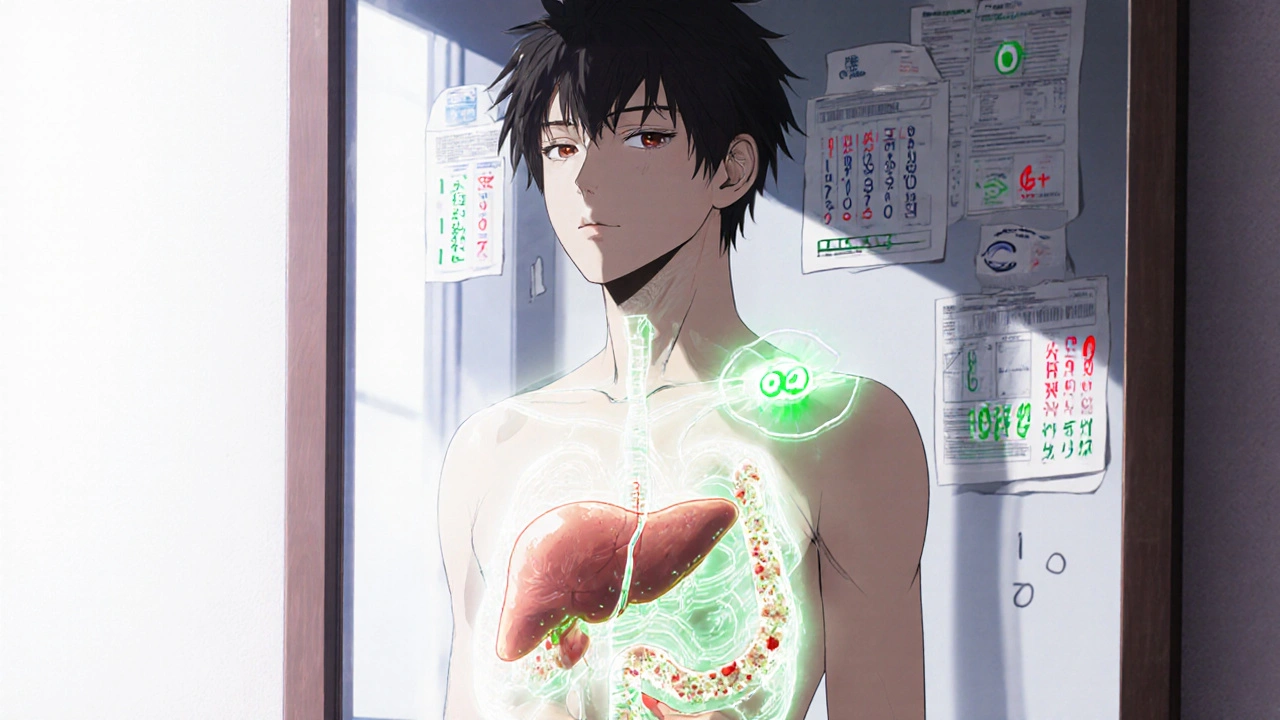
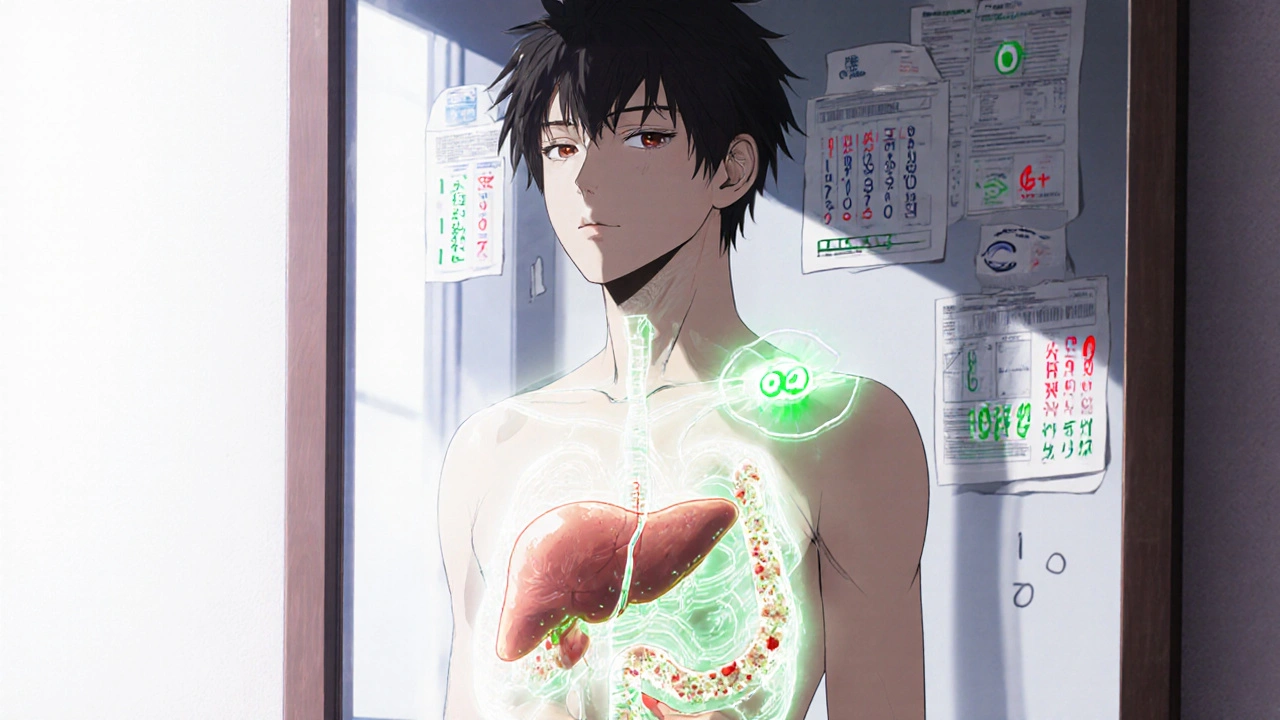
True remission means your HbA1c levels, a measure of average blood sugar over three months drop below 6.5% without using diabetes drugs for at least three months. That’s the standard set by the American Diabetes Association and confirmed by major trials like DiRECT. But it’s not just about one number. Your insulin sensitivity, how well your body responds to insulin has to improve. That’s why weight loss—especially around the liver and pancreas—is so critical. Losing even 10% of your body weight can restart insulin production in many people.
Remission doesn’t mean you’re off the hook forever. It means you’ve reset your metabolism enough to stop needing medication. But if you gain the weight back, or slip into old eating habits, diabetes can return. That’s why remission is a status, not a finish line. It’s a shift from managing a disease to maintaining a healthier version of yourself.
You won’t find remission through quick fixes. No supplement, tea, or magic pill gets you there. It’s built on consistent changes: eating fewer refined carbs, moving daily, sleeping well, and reducing stress. These are the same habits that show up in posts about diabetes medications safety, because even the best drugs can’t outwork a poor lifestyle. The science is clear: when you reduce fat in the pancreas, insulin-producing cells wake up. That’s remission in action.
Some people reach remission after bariatric surgery. Others do it with structured diet programs. A few even reverse it just by cutting out sugary drinks and walking 30 minutes a day. The path varies, but the outcome is the same: normal blood sugar without pills. And that’s powerful.
What you’ll find in the posts below isn’t theory. It’s real-world advice from people who’ve been there—how to track progress, what tests to ask for, why some medications like metformin are still used even in remission, and how to avoid slipping back. You’ll also see how kidney health, drug interactions, and even sleep patterns tie into whether remission lasts. This isn’t just about numbers on a screen. It’s about taking back control of your body—and knowing exactly what it takes to keep it.