Multiple System Atrophy: Symptoms, Causes, and Treatment Options
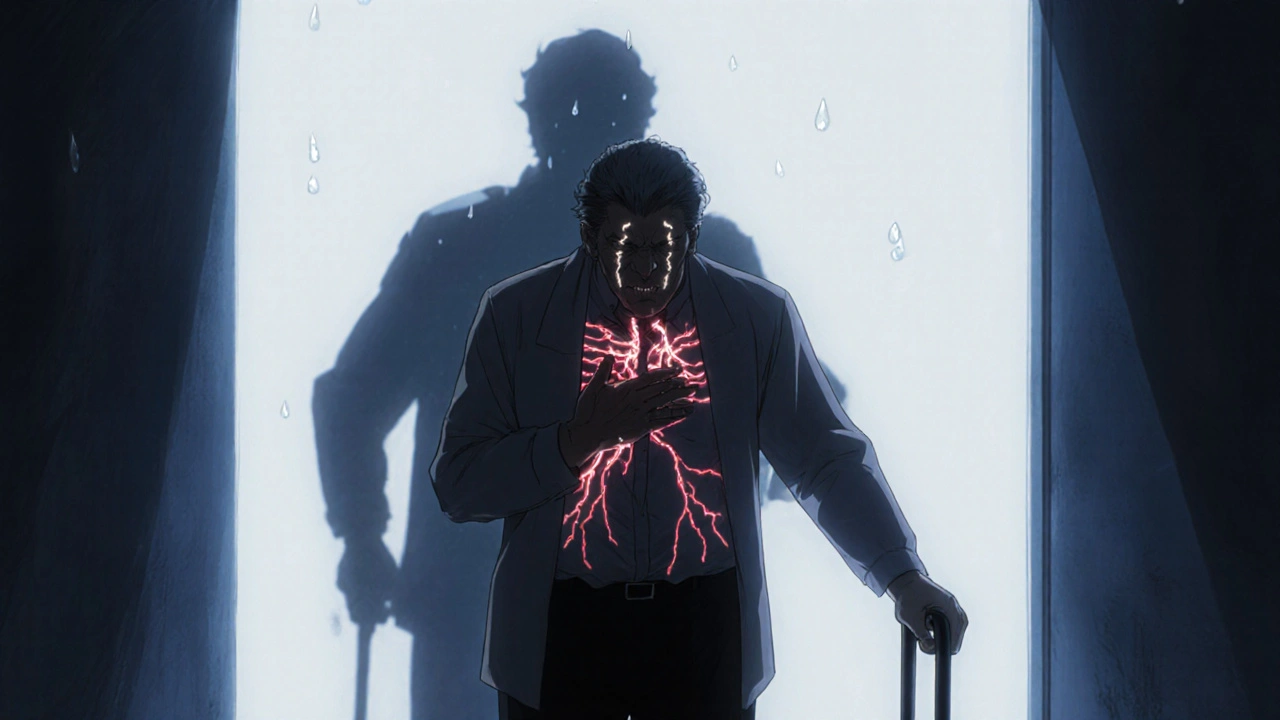
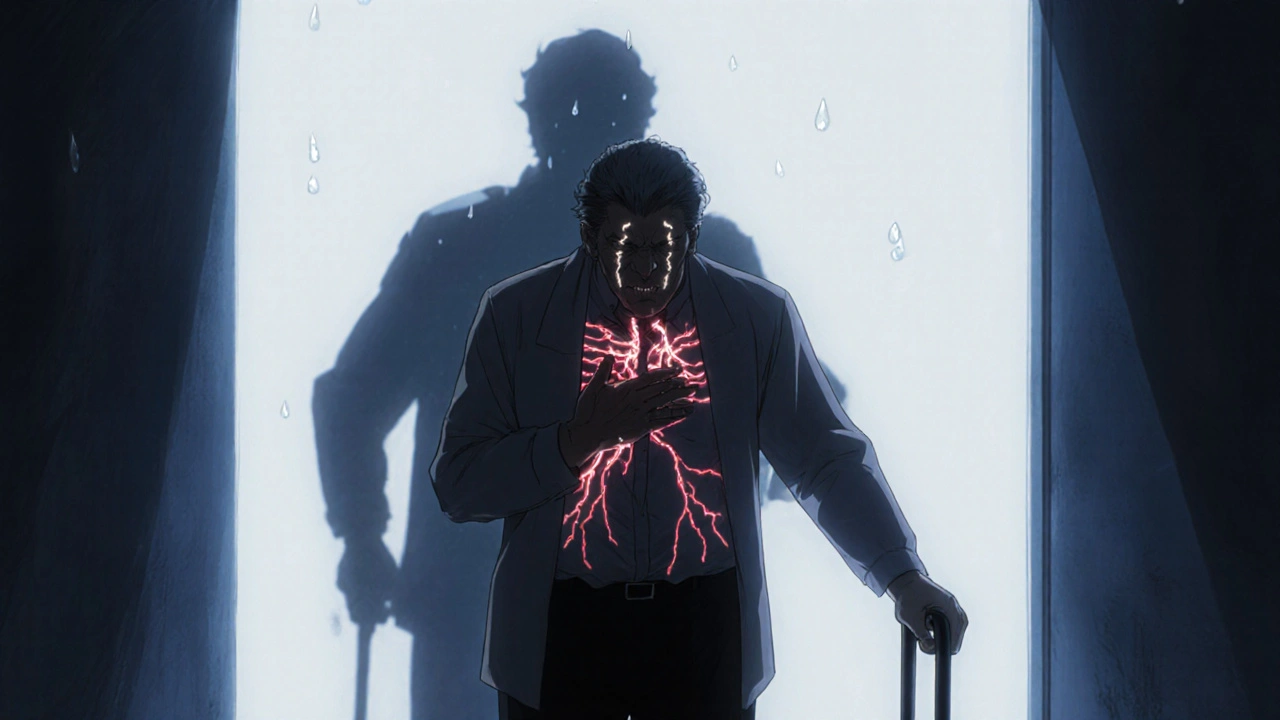
When your body starts losing control of basic functions—like standing up without dizziness, bladder control, or even swallowing—it’s not just aging. It could be multiple system atrophy, a rare, progressive neurodegenerative disorder that damages multiple parts of the nervous system, including those that control movement and automatic body functions. Also known as MSA, it’s often mistaken for Parkinson’s, but it’s faster, more aggressive, and doesn’t respond well to the same treatments. Unlike Parkinson’s, where tremors are common, MSA usually shows up as severe balance problems, rigid muscles, and sudden drops in blood pressure when you stand. This is called orthostatic hypotension, a condition where blood pressure plummets upon standing, causing fainting or near-fainting episodes. It’s not just inconvenient—it’s dangerous. People with MSA often fall without warning, and their bodies struggle to regulate temperature, heart rate, and digestion.
What makes MSA so tricky is that it attacks three systems at once: the part of the brain that controls movement (like Parkinson’s), the autonomic nervous system (which runs your heart, bladder, and digestion), and the cerebellum (which handles coordination). This is why you’ll see symptoms like slurred speech, stiff limbs, and trouble walking—even if someone has no tremors. There’s no cure, and no drug can stop it from getting worse. But levodopa, a medication commonly used for Parkinson’s disease that boosts dopamine levels in the brain, can help some people with MSA for a short time. Most won’t respond, but if they do, even a little improvement in movement can make a big difference in daily life. Other treatments focus on managing symptoms: fludrocortisone to raise blood pressure, midodrine to prevent fainting, or pelvic floor therapy for bladder issues. Sleep problems? That’s common too—many people with MSA develop sleep apnea or act out their dreams because the brain’s control over muscle movement during sleep breaks down.
There’s no blood test or scan that confirms MSA on its own. Doctors rely on a mix of symptoms, neurological exams, and ruling out other conditions like Parkinson’s or pure autonomic failure. The earlier it’s caught, the better you can plan for safety—grab bars in the bathroom, non-slip mats, voice-activated devices to avoid reaching for things. It’s not about finding a miracle cure. It’s about holding onto quality of life as long as possible. Below, you’ll find real, practical guides on medications that help, drug interactions to avoid, and how symptoms like low blood pressure or muscle stiffness are managed in people with neurodegenerative conditions. These aren’t theoretical discussions—they’re from people living with this, and the doctors who treat them every day.