PK vs PD: A Practical Guide to Pharmacokinetics and Pharmacodynamics
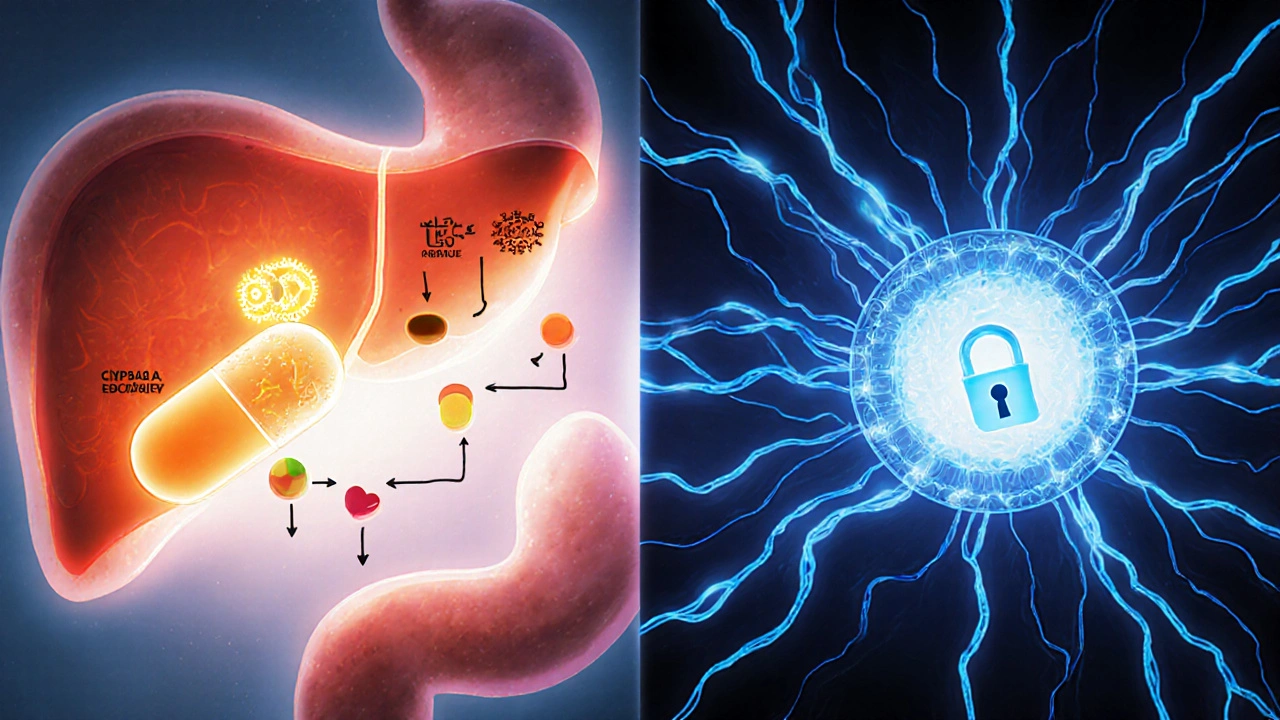
When tackling PK vs PD, the comparison between how a drug moves through the body (pharmacokinetics) and how it produces its effects (pharmacodynamics). Also known as PK/PD, this concept helps clinicians predict dosage, timing, and possible side‑effects. Understanding the link between Pharmacokinetics, the study of absorption, distribution, metabolism, and excretion (ADME) and Pharmacodynamics, the relationship between drug concentration and its biological response is essential for safe, effective therapy.
Why PK vs PD Matters in Everyday Prescribing
Most people think a prescription is just a number of pills, but the reality is far richer. PK vs PD tells us that a drug’s journey (PK) and its impact (PD) are two sides of the same coin. For instance, a medication with fast absorption may reach peak levels quickly, but if its pharmacodynamic target is slow‑acting, the therapeutic effect could lag. Conversely, a drug that hangs around in the bloodstream (high half‑life) might cause accumulation‑related side effects if its PD profile is potent. Recognizing this interplay lets you adjust doses, schedule dosing intervals, and avoid toxic peaks.
Another key player is Therapeutic Drug Monitoring, the practice of measuring drug concentrations to keep therapy within a safe and effective window. TDM bridges PK and PD by providing real‑time data on how the body handles the drug and how that translates to clinical response. When you see a patient with fluctuating blood levels, TDM helps you decide whether to tweak the dose (a PK issue) or change the drug class (a PD issue).
Drug absorption is the first step in the PK chain. Food, stomach pH, and intestinal transporters can boost or block how much of a medication actually gets into the bloodstream. Imagine taking a lipophilic antifungal on an empty stomach versus with a fatty meal – the exposure can differ dramatically, which in turn shifts the PD curve and changes efficacy. Knowing the absorption nuances lets you counsel patients on when and how to take their meds for optimal effect.
Distribution follows absorption and spreads the drug to tissues. Factors like protein binding and tissue affinity determine how much free drug reaches the target site. A highly protein‑bound drug may show low free concentrations despite high total levels, influencing its PD profile. For narrow‑therapeutic‑index drugs like warfarin, both PK (binding) and PD (bleeding risk) must be weighed carefully.
Metabolism and excretion close the PK loop. Enzyme polymorphisms (e.g., CYP2D6 poor metabolizers) can turn a standard dose into a toxic exposure, while renal impairment may slow clearance, extending the drug’s half‑life. These PK changes often manifest as altered PD outcomes – either stronger effects or more side effects. Adjusting dose or selecting alternative agents based on metabolic capacity is a core PK‑guided strategy.
Putting it all together, the PK vs PD framework is a decision‑making map. It starts with the drug’s ADME profile, moves through its mechanism of action, and ends with the clinical outcome you want. When you understand each link, you can personalize therapy, anticipate interactions, and explain the “why” behind dosing instructions. Below, you’ll find articles that dive deeper into each piece – from antifungal PK nuances to antibiotic PD comparisons – giving you concrete examples to apply this model in real‑world practice.