Skin Cancer Risk: What You Need to Know
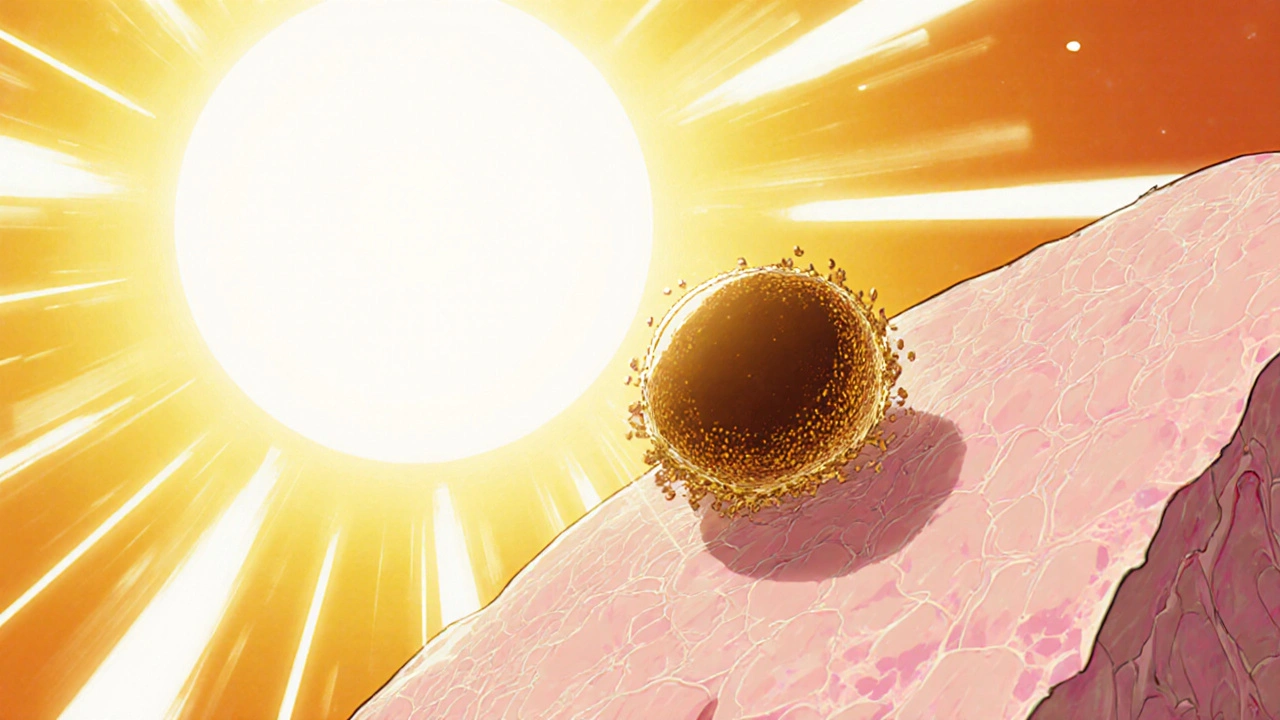
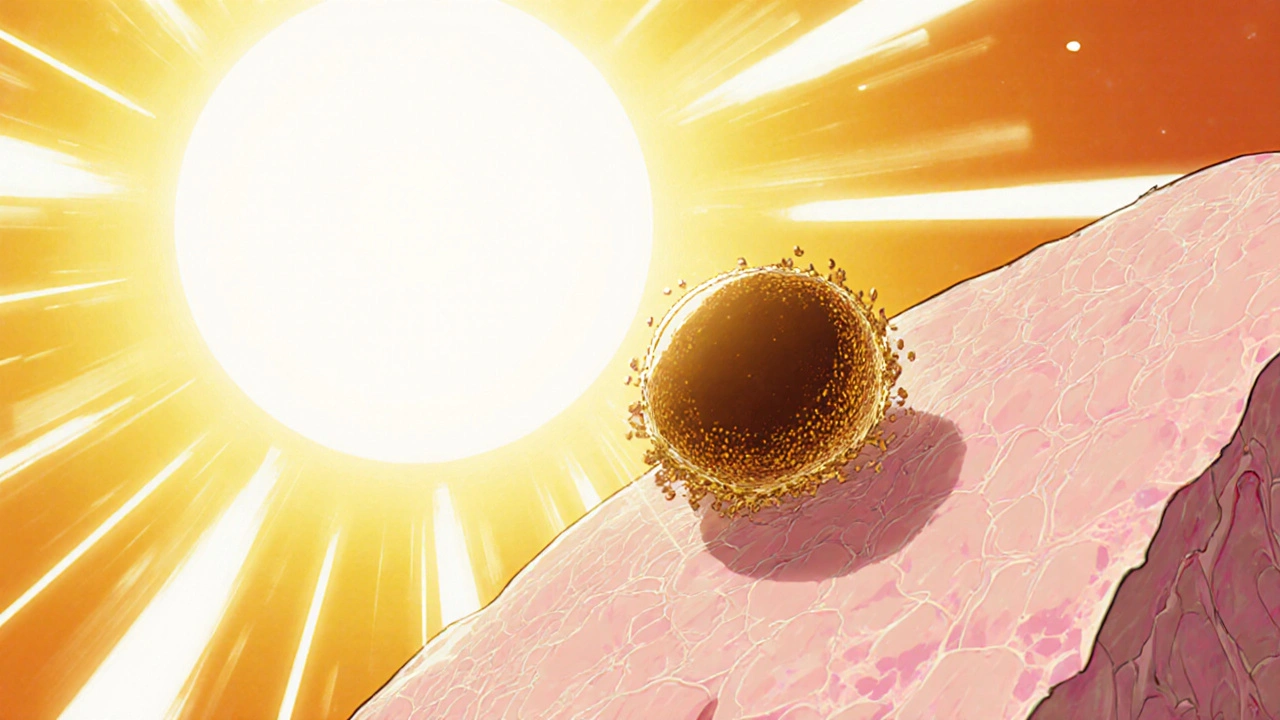
When talking about Skin Cancer Risk, the probability of developing malignant skin tumors due to environmental and personal factors. Also known as cutaneous malignancy risk, it guides how doctors assess danger and how individuals choose protection methods. Skin cancer risk is tightly linked to UV radiation, high‑energy waves from sunlight or tanning devices that damage DNA in skin cells, to the protective pigment melanin, the natural sunscreen produced by the skin that absorbs UV energy, and to the actions we take such as applying sunscreen, topical formulas that filter or block UV rays or scheduling a regular skin exam, a professional check of moles and lesions for early signs of cancer. The relationship can be summed up in simple triples: skin cancer risk encompasses UV exposure, skin cancer risk requires regular skin exams, and melanin influences skin cancer risk.
Key Factors and Prevention Tips
First, the amount of UV radiation you receive matters more than the duration alone. A 15‑minute midday walk in summer can deliver more damage than an hour in the early morning. The sun’s UVB rays are the main culprits for DNA mutations, while UVA penetrates deeper and accelerates aging. Because the skin’s natural defense – melanin – varies by ethnicity, people with lighter skin see a faster rise in risk. This explains why fair‑skinned individuals often receive more warnings about sunscreen use and skin checks.
Second, everyday protection starts with sunscreen. Choose a broad‑spectrum product with at least SPF 30, and reapply every two hours if you’re outdoors. Many forget to apply to often‑missed spots like the ears, back of the neck, and tops of the feet. Pair sunscreen with physical barriers – hats, sunglasses, and UPF clothing – and you cut the UV dose dramatically. A simple equation helps: sunscreen reduces UV penetration by a factor of the SPF number, while clothing can block up to 90 % of UV rays.
Third, regular skin exams catch problems before they spread. A self‑exam once a month, looking for new or changing moles using the ABCDE rule (Asymmetry, Border, Color, Diameter, Evolving), tells you when to see a dermatologist. Professional exams once a year add a second set of eyes and may include dermatoscopic imaging for deeper analysis. Early detection raises the five‑year survival rate for melanoma from about 65 % to over 95 %.
Beyond UV and skin checks, lifestyle choices affect the overall risk profile. Smoking, for example, weakens immune surveillance, making it harder for the body to clear abnormal cells. A diet rich in antioxidants – vitamins C and E, selenium, and leafy greens – can repair some DNA damage caused by UV exposure. Physical activity improves circulation, which supports the skin’s natural repair mechanisms.
Genetics also play a role. Family history of melanoma, many atypical moles, or conditions like xeroderma pigmentosum dramatically increase the baseline risk. If you fall into any of these categories, your doctor may recommend more frequent exams or even genetic counseling. Knowing your personal risk lets you tailor prevention: stronger sunscreen, stricter sun‑avoidance schedules, and earlier specialist visits.
All of these angles – UV exposure, melanin levels, sunscreen habits, skin exams, lifestyle, and genetics – weave together to define a person’s skin cancer risk. Below you’ll find a collection of articles that dive deeper into each piece, from practical guides on choosing the right sunscreen to the science behind DNA repair after sun damage. Use them as a toolbox to lower your risk and stay ahead of potential problems.